ORIGINAL RESEARCH ARTICLE
Measures of Well-Being in U.S. Animal Shelter Staff During 2023
Peter J. Wolf1, Maureen Gillespie1 and Chris Segrin2
1Best Friends Animal Society, Kanab, UT, USA; 2Department of Communication, University of Arizona, Tucson, AZ, USA
Abstract
Introduction: The demands of animal shelter work can take a toll on staff well-being. The years following the coronavirus pandemic have been especially demanding as shelters struggle to navigate a series of unprecedented challenges, including pandemic-related restrictions, the shortage of veterinary professionals, adoptions not keeping pace with increasing animal admissions (especially of dogs), the expiration of eviction moratoriums, and rising inflation. These factors create a context that is potentially deleterious to the well-being of shelter staff.
Methods: We used an online survey to collect information from U.S. shelter staff (N = 243). Specifically, we used the Patient-Reported Outcomes Measurement Information System (PROMIS) and Professional Quality of Life (ProQOL) instruments to quantify various aspects of staff well-being. We also collected basic demographic information and details about participants’ experience in the animal welfare field.
Results: PROMIS results reveal mean anger, anxiety, depression, and fatigue scores in the mild/moderate range, significantly higher than those of the general U.S. population. ProQOL results show that nearly half of shelter staff respondents (49.4%) recorded compassion satisfaction scores in the high range, with the remainder falling into the moderate (39.1%) or low (11.5%) range; 53.5% recorded burnout scores in the high range, with the remainder falling into the moderate (32.1%) or low (14.4%) range; and 90.9% recorded secondary traumatic stress scores in the high range, with the remainder falling into the moderate (8.2%) or low (0.8%) range.
Conclusion: Although the shelter staff surveyed reported high levels of job satisfaction, their high burnout and secondary traumatic stress scores, and lower mental and physical health scores raise serious concerns about employee well-being and potential turnover following the coronavirus pandemic. If much of the trauma that comes with animal sheltering work cannot be avoided, policymakers should consider providing shelter staff with the resources necessary to mitigate its impact.
Keywords: animal shelters; burnout; compassion fatigue; COVID-19; PROMIS; ProQOL; well-being
Citation: Journal of Shelter Medicine and Community Animal Health 2024, 3: 81 - http://dx.doi.org/10.56771/jsmcah.v3.81
Copyright: © 2024 Peter J. Wolf et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 12 February 2024; Revised: 12 September 2024; Accepted: 12 September 2024; Published: 18 October 2024
Competing interests and funding: In recognition of JSMCAH policy and our ethical obligations as researchers, the authors acknowledge that two of us are employed by a national animal welfare organization that promotes programs and policies to increase lifesaving in animal shelters across the United States. No external funding was provided for this research.
Corresponence *Peter J. Wolf, 5001 Angel Canyon Road, Kanab, Utah, 84741. Email: peterw@bestfriends.org
Reviewers: Maya Gupta, Aimee Dalrymple
Supplementary material: Supplementary material for this article can be accessed here.
Much of the information provided here was first published and posted on the BFAS website in September 2023.
Animal shelter work encompasses a broad range of tasks and responsibilities; some roles involve direct animal care (e.g. kennel attendant and field services officer), whereas others are more administrative in nature (e.g. adoption coordinator and executive director). Each of these roles likely has its own stresses – those of an adoption coordinator being different from those of a shelter’s field services staff, for example. In some shelters, especially in smaller agencies, staff often fill multiple roles, subjecting themselves to the stresses associated with each role. But even in the largest shelters, where roles and responsibilities are more narrowly defined, the pressure to provide the best outcome for each animal in one’s care is likely felt by all shelter staff.
Animal shelter work is demanding, and, not surprisingly, these demands can take a toll on staff well-being. The years following the coronavirus pandemic have been especially demanding, as shelters struggle to navigate a series of unprecedented challenges, including pandemic-related restrictions,1 the shortage of veterinary professionals,2 adoptions not keeping pace with increasing animal admissions (especially of dogs),a the expiration of eviction moratoriums,3 and rising inflation.4
Shelter staff well-being was conceptualized with two superordinate constructs, each with its attendant sub-dimensions. The first component of staff well-being was psychological quality of life. The derivative domains of psychological quality of life included both positive (i.e. self-efficacy, companionship, emotional support, informational support, and satisfaction with roles and activities) and negative (i.e. anger, anxiety, and depression) indicators, as indexed by the Patient-Reported Outcomes Measurement Information System (PROMIS).5 The positive indicators reflect a sense of feeling connected and supported socially, contentment and enjoyment with activities, and feeling able to affect outcomes in one’s own life. The negative indicators reflect experiences of bothersome negative affect. Measures of these and other PROMIS domains were developed using item response theory approaches to calibrate test item banks and generate a scoring system that establishes norms within the general U.S. population.6,7 The second component of well-being assessed in this investigation was professional quality of life. Stamm8 defines professional quality of life as ‘the quality one feels in relation to their work as a helper’. Like psychological quality of life, professional quality of life has multiple domains, the first of which is compassion satisfaction (CS). People high in CS derive substantial pleasure from being able to perform their work helping others. The second domain is compassion fatigue, which is indexed by two indictors: burnout (BO) and secondary traumatic stress (STS). People who feel burned out feel exhausted, frustrated, hopeless, and angry because of their work. STS is the result of working with others who have experienced traumatic and stressful events in the workplace. This secondary traumatic exposure is hypothesized to generate fear, intrusive images or thoughts, and sleep disruption. Professional quality of life was assessed with the ProQOL instrument,8 which has been widely and successfully used throughout the helping professions,9–14 including animal care workers.15–20
To our knowledge, the PROMIS measures have not been used to assess shelter staff well-being. However, they have generally demonstrated good validity21 and were attractive for the present study largely because of their extensive prior use in other fields, allowing for comparisons to nationally normed data. The ProQOL, first introduced in 2005,22 was based on the Compassion Fatigue Self Test developed 10 years earlier for psychotherapists.23 The instrument was quickly adopted for use in studies of nurses and other healthcare providers.24–26 Later, it was adopted by researchers studying veterinary professionals and others caring for animals.27,28 Among the first to use ProQOL to assess the well-being of animal shelter staff were Rank et al., who used the instrument to assess the effectiveness of a ‘compassion fatigue training module’.16
Although several studies have examined the well-being of animal shelter staff,16,18,19,29–31 the results of one sometimes contradict those of another. The authors of a 2015 study found, for example, that ‘personnel directly engaged in euthanasia reported significantly higher levels of work stress and lower levels of job satisfaction, which may have resulted in higher employee turnover, psychological distress, and other stress-related conditions’.31 However, other studies have found that factors other than direct involvement with euthanasia contribute more to job-related stress.19,32,33 In addition, the results of a single survey can sometimes be counterintuitive. One recent study found that staff working in shelters with higher live-release rates (LRRs) reported greater levels of CS (i.e. the pleasure derived from being able to help others through their work) while also reporting higher levels of some work-related stress (e.g. BO and STS) than those in shelters with lower LRRs. These seemingly contradictory findings led the researchers to conclude that staff in shelters with higher LRRs feel ‘that they are making more of a difference and are helping more animals’ – but also feel an ‘increased hopelessness in their work’.19
The purpose of the present study was to investigate animal shelter staff well-being across the United States in the wake of the coronavirus pandemic, adding to this important area of research. In particular, we aimed to answer the following questions:
- How does current shelter staff well-being compare to that of the general public?
- How does current shelter staff well-being compare to that of individuals employed in other ‘helping professions’ (e.g. nurses and first responders)?
- To what extent might current levels of staff well-being correlate with key shelter metrics (e.g. annual animal intake, LRR)?
Methods
We used an online survey for this cross-sectional study of animal shelter staff well-being, collecting participants’ demographic and employment information, as well their responses to standardized measures of well-being. The complete survey is available in the Supplementary material.
Recruitment
Recruitment was done primarily through e-mail communication from Best Friends Animal Society (BFAS) to the organization’s Network partners, a collection of more than 4,400 shelters and rescue groups across the country who regularly share their data with BFAS. Additional recruitment was done through social media (e.g. a Facebook group open only to BFAS Network partners) and e-mail communication facilitated by the National Animal Care & Control Association. The survey was available online, via Qualtrics (April–June 2023), from April 5 through June 8, 2023.
Participation was limited to paid staff of U.S. brick-and-mortar shelters and was entirely voluntary. A $5 Amazon gift card code was sent to participants who shared their e-mail address and completed a survey. Respondents were free to quit the survey at any point and were able to skip any question that they did not wish to answer. All responses were anonymous. The research protocol was reviewed and approved by the Institutional Review Board at the University of Arizona under protocol number MOD00003395.
Measures
The survey was comprised of 3 sections: (1) a series of questions to collect participants’ demographic and employment information, (2) the PROMIS scale,5 and (3) the ProQOL scale.8 Mental, physical, and social health were assessed using 9 PROMIS scales: anger, anxiety, depression, self-efficacy, fatigue, companionship, emotional support, informational support, and satisfaction with roles and activities. Associated categories of well-being, number of items per scale, and alpha reliabilities appear in Table 1. All PROMIS items used for the present study were responded to using a 5-point Likert scale (1 = never, 2 = rarely, 3 = sometimes, 4 = often, and 5 = always; or 1 = not at all, 2 = a little bit, 3 = somewhat, 4 = quite a bit, and 5 = very much). Raw PROMIS scores were converted to T-scores so that they could be compared to those of the general U.S. adult population (i.e. mean = 50, standard deviation [SD] = 10). Participants’ scores were calculated using the online HealthMeasures Scoring Service.34
Professional quality of life was assessed with the ProQOL instrument so that shelter staff scores could be compared with those of others employed in the helping professions. The instrument’s extensive application in surveys of helpers (including animal shelter staff18,19) made it an attractive choice for the present study. The ProQOL instrument is made up of 30 Likert-scale items broken into two primary components: CS and compassion fatigue, with compassion fatigue being made up of 2 components: BO and STS.
Some items were modified to better fit animal shelter staff (e.g. ‘I get satisfaction from being able to [help] people’ was modified to ‘I get satisfaction from being able to help animals’), as shown in Table S1. Each of the 3 ProQOL components was scored separately by summing the appropriate 10 items using a 5-point system (1 = never, 2 = rarely, 3 = sometimes, 4 = often, and 5 = very often). For BO scores, 5 of the 10 items were first reverse-coded. Alpha reliabilities for each scale appear in Table 2. Following previous research,35 we used mean substitution for missing values. Although this method is biased toward the mean,36 it was justified in this case because the percentage of missing data for each ProQOL item ranged from 0 to 0.8% making the potential effect of this imputation negligible. Following De La Rosa et al.,37 we adopted the low, moderate, and high thresholds for each of the 3 ProQOL components, as described in Table 2.
Data cleaning
During initial recruitment efforts, 221 valid responses (90.1% of the total) were received, after which 2 bot attacks occurred (the apparent result of the survey being posted to at least 1 social media platform). Just 6 of 721 submissions (0.8%) from the first attack and 16 of 235 submissions (6.8%) from the second attack were deemed valid and retained for analysis.
The details of how we addressed concerns over this threat to data quality are described in Appendix A.
Statistical analysis
The pattern of missingness in the data file was evaluated with the Missing Completely at Random test in SPSS 28.0 and found to be missing completely at random (χ2 = 1427.38, df = 1403, P = 0.319). For all quantitative variables, data were missing in 0–2.1% of the cases. Descriptive statistics were then calculated for respondents’ PROMIS and ProQOL scores using Excel (Microsoft Corporation, version 2307). Analyses of Variance (ANOVAs) were used to determine if ProQOL scores varied significantly by organization type (e.g. municipal vs. private shelter). Because annual intake and LRR data were not normally distributed, we used Spearman’s rank correlation coefficients to determine the extent to which ProQOL scores were related to annual intake or LRR. The Asilomar version of LRR38 (i.e. live outcomes divided by [all outcomes minus unhealthy/untreatable owner-requested euthanasia]) was used so that our results could be compared with those reported in a previous study.19 To account for multiple comparisons, the Benjamini-Hochberg Procedure was used to adjust P-values.39 T-tests were used to compare mean PROMIS T-scores to the U.S. population (mean 50, SD 10) and to compare ProQOL scores of shelter staff hired before and after 2020. All statistical analyses were conducted using RStudio (version 4.2.2). P-values < 0.05 were considered statistically significant.
Results
Results are reported in accordance with the Enhancing the QUAlity and Transparency Of health Research (EQUATOR) Network’s Checklist for Reporting Of Survey Studies (CROSS),40 where applicable. A total of 243 shelter staff members from 122 shelters completed the survey. Staff employed by municipal shelters made up 22.2% of our sample, while the remainder were employed by private shelters with government contracts (34.2%) or private shelters without contracts (37.4%). Private shelters are therefore overrepresented in our sample (Table 3).
| Shelter type | Number (%) | ||
| Present study | U.S. shelters | ||
| (participants) | (shelter type) | ||
| Municipal | 54 (22.2) | 34 (27.9) | 2,175 (55.3) |
| Private shelter with contract(s) | 83 (34.2) | 43 (35.2) | 845 (21.5) |
| Private shelter without contract(s) | 91 (37.4) | 45 (36.9) | 910 (23.2) |
| Other* | 15 (6.2) | – | – |
| Total | 243 (100) | 122 (100) | 3,930 (100) |
| * No shelter name provided or not included in BFAS database. U.S. shelter data compiled by BFAS. | |||
Shelter staff who identify as women and/or White made up 84.8 and 93.8% of our sample, respectively. This generally agrees with data from the U.S. Bureau of Labor Statistics for ‘animal caretakers’, indicating that 76.0% identify as women and 87.8% identify as White.41 Respondent demographics are provided in Table 4, and employment details are provided in Table 5.
| Demographic category | n (%) |
| Gender identity (N = 243) | |
| Male | 26 (10.7) |
| Female | 206 (84.8) |
| Non-binary | 7 (2.9) |
| Transgender | 2 (0.8) |
| Other | 1 (0.4) |
| Prefer not to say | 1 (0.4) |
| Age (N = 243) | |
| 18–25 | 33 (13.6) |
| 26–35 | 68 (28.0) |
| 36–45 | 67 (27.6) |
| 46–55 | 31 (12.8) |
| 56–65 | 37 (15.2) |
| >65 | 7 (2.9) |
| Prefer not to say | 0 (0.0) |
| Race* (N = 243) | |
| White | 228 (93.8) |
| Black or African American | 4 (1.6) |
| American Indian or Alaska Native | 3 (1.2) |
| Asian | 9 (3.7) |
| Native Hawaiian or other Pacific Islander | 1 (0.4) |
| Some other race | 6 (2.5) |
| Prefer not to say | 1 (0.4) |
| Ethnicity (N = 241) | |
| Hispanic or Latino | 19 (7.9) |
| Not Hispanic or Latino | 219 (90.9) |
| Prefer not to say | 3 (1.2) |
| Level of education (N = 243) | |
| No formal educational credential | 1 (0.4) |
| High school diploma or equivalent | 20 (8.2) |
| Some college, no degree | 52 (21.4) |
| Postsecondary nondegree award | 4 (1.6) |
| Associate degree | 37 (15.2) |
| Bachelor’s degree | 82 (33.7) |
| Master’s degree | 39 (16.0) |
| Doctoral or professional degree | 6 (2.5) |
| Prefer not to say | 2 (0.8) |
| Marital status (N = 243) | |
| Never married | 67 (27.6) |
| Married | 101 (41.6) |
| Living with a partner | 40 (16.5) |
| Separated | 2 (0.8) |
| Divorced | 26 (10.7) |
| Widowed | 5 (2.1) |
| Prefer not to say | 2 (0.8) |
| Parent/caregiver (N = 243) | |
| Yes | 83 (34.2) |
| No | 159 (65.4) |
| Prefer not to say | 1 (0.4) |
| Current financial situation (N = 242) | |
| Cannot get by without assistance | 10 (4.1) |
| Struggling to get by | 17 (7.0) |
| Just getting by | 89 (36.8) |
| Able to get by with a little left over | 89 (36.8) |
| Able to get by very comfortably | 37 (15.3) |
| * More than one choice allowed. | |
| Employment information | n (%) |
| Shelter type (N = 243) | |
| Municipal | 54 (22.2) |
| Private shelter with contract(s) | 83 (34.2) |
| Private shelter without contract(s) | 91 (37.4) |
| Unlisted shelters | 4 (1.6) |
| Anonymous* | 11 (4.5) |
| Position at shelter† (N = 243) | |
| Management | 135 (55.6) |
| Operations, admissions | 45 (18.5) |
| Operations, adoptions | 49 (20.2) |
| Operations, animal care | 62 (25.5) |
| Operations, medical | 38 (15.6) |
| Administrative (e.g. data entry) | 34 (14.0) |
| Other | 51 (21.0) |
| Time in current position (N = 243) | |
| < 1 year | 44 (18.1) |
| 1–3 years | 100 (41.2) |
| 4–6 years | 56 (23.0) |
| 7–10 years | 20 (8.2) |
| 11–15 years | 13 (5.3) |
| > 15 years | 10 (4.1) |
| Time at shelter (N = 243) | |
| < 1 year | 27 (11.1) |
| 1–3 years | 89 (36.6) |
| 4–6 years | 55 (22.6) |
| 7–10 years | 26 (10.7) |
| 11–15 years | 24 (9.9) |
| >15 years | 22 (9.1) |
| Intent to continue working at this shelter for the foreseeable future (N = 242) | |
| Very likely | 181 (74.8) |
| Somewhat likely | 48 (19.8) |
| Not likely | 13 (5.4) |
| Position(s) in animal welfare field† (N = 243) | |
| Shelter staff (paid) | 217 (89.3) |
| Enforcement/field services | 21 (8.6) |
| Rescue organization staff | 21 (8.6) |
| Shelter or rescue volunteer | 3 (1.2) |
| Other | 10 (4.1) |
| Time in animal welfare field (N = 242) | |
| <1 year | 17 (7.0) |
| 1–3 years | 58 (24.0) |
| 4–6 years | 54 (22.3) |
| 7–10 years | 35 (14.5) |
| 11–15 years | 35 (14.5) |
| >15 years | 43 (17.8) |
| * Assumed to be shelters. | |
| † More than one choice allowed. | |
RQ1: Comparing shelter staff well-being to that of the general public
The mental health of this sample of shelter workers is characterized by not only significantly more anger, depression, and anxiety compared to that of the general population but also significantly higher self-efficacy (Fig. 1). The physical health of this sample is characterized by significantly greater fatigue than that of the general population. In terms of social well-being, participants reported significantly greater informational support but significantly lower satisfaction with social roles compared to population norms. The sample of shelter workers was comparable to the generation population on measures of companionship and emotional support.
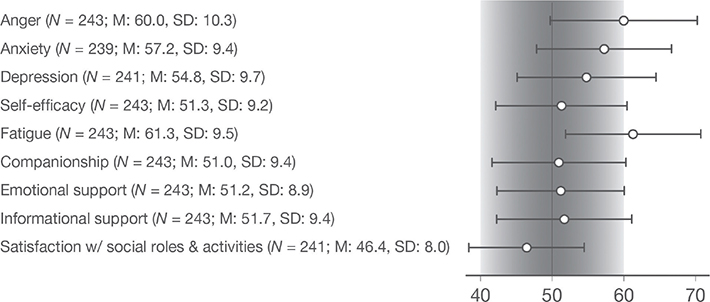
Fig. 1. Summary of PROMIS scores. Shaded area represents standardized scores of U.S. adult population (M: 50, SD: 10). For anger, anxiety, depression, and fatigue, higher stores indicate lower levels well-being; for self-efficacy, companionship, emotional support, informational support, and satisfaction with social roles & activities, higher scores indicate greater levels well-being.
RQ2: Comparing shelter staff well-being to that of other helping professions
CS, BO, and STS scores were calculated for each respondent who completed the survey. Descriptive statistics are provided in Fig. 2.
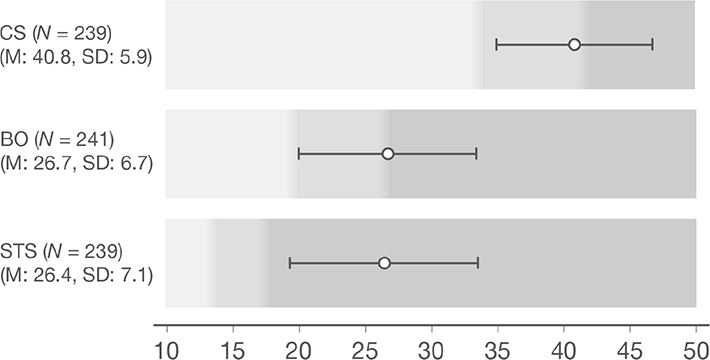
Fig. 2. Summary of ProQOL scores. Shaded areas represent low, moderate, and high ranges of each component, as suggested by De La Rosa et al.37 Specifically, compassion satisfaction (CS): ≤ 33 = low, 34–41 = moderate, and ≥ 42 = high; burnout (BO): ≤ 19 = low, 20–26 = moderate, and ≥ 27 = high; secondary traumatic stress (STS): ≤ 13 = low, 14–17 = moderate, and ≥ 18 = high. Note: Descriptive statistics calculated using mean substitution for missing values, N = 243.
Nearly half of shelter staff respondents (49.4%) recorded CS scores in the high range, with the remainder falling into the moderate (39.1%) or low (11.5%) range. More than half our respondents (53.5%) recorded BO scores in the high range, with the remainder falling into the moderate (32.1%) or low (14.4%) range. Roughly 9 in 10 of our respondents (90.9%) recorded STS scores in the high range, with the remainder falling into the moderate (8.2%) or low (0.8%) range. No statistically significant differences were found between ProQOL scores and shelter type (e.g. municipal vs. private) with all Fs < 2.0 and all Ps > 0.12.
Nearly three quarters of respondents (74.8%) indicated that they are likely to continue working at the shelter currently employing them, while the remainder indicated that they are either somewhat likely (19.8%) or unlikely (5.4%) to continue. Shelter staff reporting higher BO scores were significantly less likely to continue working at the shelter where they are currently employed compared to staff reporting lower BO levels (t(240) = 7.10, P < 0.001, Fig. 3). A similar trend was observed for STS scores (t(240) = 4.36, P < 0.001).
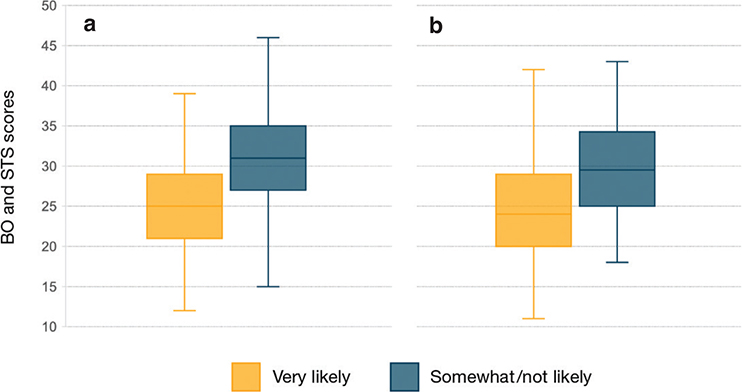
Fig. 3. Burnout (BO) and secondary traumatic stress (STS) scores. BO scores (a) for shelter staff indicating that they were very likely to continue working at their current shelter (mean 25.1, SD 6.1) compared to those indicating that they were either somewhat likely or not likely to continue (mean 31.5, SD 6.0). Boxes are bounded by 25th and 75th quartiles with horizontal bars indicating the medians. Whiskers indicate minimum and maximum values. STS scores (b) show a similar trend (very likely: mean 25.3, SD 7.0; somewhat/not likely: mean 29.8, SD 6.6). For both BO and STS, higher stores indicate lower levels well-being.
We compiled means and standard deviations from 3 investigations of helping professions that used the PROMIS anger, depression, anxiety, or fatigue measures42–44 and 19 investigations that used the ProQOL measures.10–14,16,18,19,29,45–54 Means from these investigations were compared to relevant means from the present sample using Welsh’s t-tests due to the differing sample sizes across the various comparisons (Table S2). The results show that with few exceptions, the present sample of animal shelter staff scored higher on indicators of distress such as anger, depression, anxiety, fatigue, BO, and STS when compared to groups such as nurses, law enforcement, laboratory animal technicians, and ocean lifeguards. It should be noted, however, that many of these previous studies were conducted prior to the coronavirus pandemic, which might account for some of the differences seen in our comparisons.
RQ3: Shelter staff well-being and shelter metrics
The median LRR for shelters responding to our survey was 94% (range: 52–100%); median annual intake was 2,394 animals (range: 45–33,916). To examine the relationship between shelter staff well-being and these shelter metrics, all PROMIS and ProQOL measures were correlated with yearly shelter intake and LRR, data available for 200 of our respondents. No significant correlations were found between PROMIS or ProQOL measures and LRR or intake (Table 6).
We found no significant differences between CS or STS scores of staff who have been involved with animal welfare work for 3 years or less and scores of staff with 4 or more years of experience, t(240) = 0.34, P = 0.73 and t(240) = −0.04, P = 0.97, respectively. We did, however, observe a relatively minor difference between their BO scores, with staff hired post-pandemic reporting slightly lower BO scores those hired pre-pandemic (t(240) = −1.69, P = 0.09).
Discussion
The specific aims of this study were to compare the well-being of animal shelter staff workers to that of the general population as well as those in other helping professions. Additionally, we sought to determine whether the nature of shelter work, specifically intake volume and LRR, was associated with shelter worker well-being. To our knowledge, our sample (243 shelter staff members from 122 shelters) makes this the largest survey of its kind to date. The results showed that shelter workers reported significantly higher anger, anxiety, depression, and fatigue compared to the general population. Over half of the respondents reported high levels of BO and STS. Animal shelter workers also scored higher on indicators of distress such as anger, depression, anxiety, fatigue, BO, and STS when compared to other people employed in the helping professions. Finally, the nature of shelter work, as indexed by intake volume and LRR, was not associated with any measure of shelter worker well-being.
Shelter worker well-being
The mean CS score observed is considered moderate to high,37 comparable to scores reported by shelter staff in other studies,18,19,29 notably higher than those reported in some studies of veterinary professionals,48 and slightly higher than those reported in some studies of critical care medical professionals14,53,55 and child protection workers.11,54 By contrast, higher CS scores were reported in studies of ocean lifeguards,12 former and current dog fosters,52 foster parents (of children) in the UK,47 and ‘mental health professionals treating military service members with combat trauma’.49
As noted previously, just over half of the respondents recorded BO scores in the high range,37 with the remainder falling into the moderate or low range. Over 90% recorded STS scores in the high range, with the remainder falling into the moderate or low range. Although moderate and high scores were not entirely unexpected, the STS scores in particular are among the highest observed in the published literature.
The level of BO reported by our participants is comparable to levels reported by shelter staff in some studies18,19 but slightly higher than those reported in another.29 The scores we observed were also comparable to those reported by studies of veterinary professionals,48 medical trainees learning surgical techniques,56 and ‘full-time police officers in the northwest of England, U.K. with no previous diagnosis of PTSD’.46 Interestingly, BO levels among the shelter staff we surveyed were comparable to55 or exceeded those reported by critical care medical professionals.14,53
The mean STS score we observed was well above the threshold to be considered high,37 and exceeding those reported by shelter staff in other studies.18,19,29 Indeed, the STS levels reported by the shelter staff we surveyed exceeded most of those reported in the published literature, including from studies of critical care medical professionals14,53 (with at least one exception55), child protection workers,11,54 and therapists working with survivors of sexual violence and other trauma survivors.35 One of the few studies reporting comparable STS values involved veterinary professionals.48
An unusual combination of high CS and STS scores
A comparison of CS and STS scores reveals an interesting relationship, with 42.8% of respondents scoring in the high range for both CS (≥ 42) and STS (≥ 18). This combination of high CS and high STS scores sets our sample of shelter staff apart from other helping professions. Of the 20 studies whose results are illustrated in Fig. 4, only one reported higher CS and STS scores. This was a study of adults in the U.K. caring for foster children,47 including those expressing a strong interest in continuing this work (46a) and those with ‘low intent’ (46b). The CS and STS scores we observed exceed the mean scores reported by Andrukonis and Protopopova19 (CS: 39.8, STS: 22.7) and Scotney et al.29 (CS: 39.2, STS: 29.6), and only slightly exceed those reported recently by Andrukonis et al.17 (CS: 40.4, STS: 25.9), the 3 studies most similar to ours (i.e. involving shelter staff). The study with CS and STS scores closest to those we observed among shelter staff (30) comes from a study of healthcare frontline providers deployed by non-governmental organizations to work with Ebola patients in West Africa between 2014 and 2015.51 Although the stresses associated with these vastly different jobs are likely quite different, the associated well-being scores (via the ProQOL instrument) are surprisingly similar.
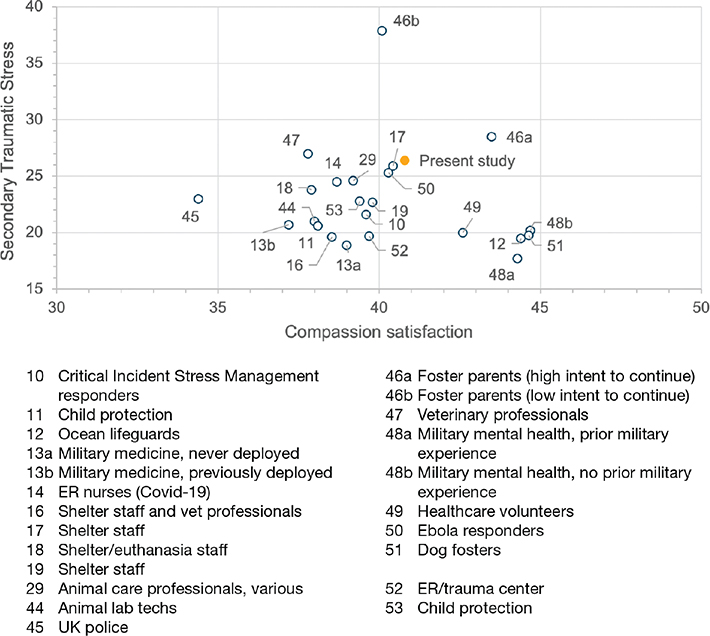
Fig. 4. Mean compassion satisfaction (CS) and secondary traumatic stress (STS) scores from various studies. The solid dot indicates scores for U.S. shelter staff from the present study. Numbers refer to the publications cited throughout. For CS, higher stores indicate greater levels well-being; for STS, higher stores indicate lower levels well-being.
Others have suggested that the ‘compassion framework’ is a ‘response continuum of work-related stress ranging from fatigue to satisfaction’, challenging the notion that individuals can truly score high on both CS and STS scales.11 The findings from this study, as illustrated in Fig. 4, suggest otherwise. However, it is not clear why animal shelter work might lead to ProQOL results so different from those associated with other helping professions. If it is true that high levels of CS are integral to animal sheltering work, this may lead staff to experience – and tolerate – high levels of both BO and STS. This would seem to have policy implications; specifically, if much of the trauma that comes with animal sheltering work cannot be avoided, it is important that shelter staff has access to techniques and programming that can mitigate its impact.
Shelter admissions and live-release rates
Annual intake and LRRs were of particular interest to us; this was in part because of previous research on the subject. A 2017–2018 survey of U.S. shelter staff revealed significant positive correlations between LRRs and BO, CS, and STS scores.19 However, our results revealed no such correlations (Table 6). There are a number of possible explanations for the differences in the results of the two surveys. For example, the median LRR for the shelters included in the earlier survey was 81%, compared to a median LRR of 94% for shelters responding to our survey. And the range of LRRs in the earlier survey was wider (i.e. 25–98% vs. 52–100%). Restriction of range will attenuate observed relationships between quantitative variables. In addition, our survey was conducted well after the beginning of the COVID-19 pandemic, at a time when there might have been a shift in these relationships (e.g. resulting from a steady increase in admissions following pandemic restrictions). In any case, the 2 results are not necessarily in conflict. It makes sense, for example, that staff working in shelters with higher rates of lifesaving can experience both higher CS (from their many lives saved) and STS scores (as each life lost is felt more acutely).
Potential impact of COVID-19 pandemic
It is virtually impossible to examine shelter staff well-being in 2023 without considering the possible effects of the COVID-19 pandemic and the ‘great resignation’. However, we found no significant differences between CS or STS scores of staff who had been involved with animal welfare work for 3 years or less and scores of staff with 4 or more years of experience. We did, however, observe a relatively minor difference between their BO scores, with staff hired post-pandemic experiencing slightly less BO than those hired pre-pandemic.
As noted previously, the CS and STS scores we observed are higher than the mean scores reported in 2 previous studies of shelter staff.19,29 It is worth noting that both of these studies were conducted prior to the coronavirus pandemic. However, the extent to which this explains the difference in scores, if at all, remains unclear.
Potential impact on staff turnover
There is evidence to show that feeling passionate about one’s work – generally considered a positive attribute, especially in the animal welfare field – can itself contribute to BO.57 We saw the potential impact of BO when we asked respondents how likely they were to continue working at their current shelter for the foreseeable future. The mean BO score for those indicating that they were very likely to stay was 25.1 (SD 6.1), considerably lower than the mean (31.6, SD 6.0) for those indicating that they were somewhat likely or unlikely to stay. A similar trend was seen for STS scores (Fig. 1). These findings correspond with those from other studies of the helping professions showing that as staff well-being decreases, the likelihood of turnover increases. A study of child therapists in Norway, for example, found that respondents with higher BO and STS scores expressed a ‘higher intention to leave’ than those with lower BO and STS scores.58 A study of oncology nurses in the United States found a statistically significant relationship between BO scores and turnover intent, but not between STS scores and turnover intent.59 A large-scale survey of academic physicians (N = 18,719), which used PROMIS to measure anxiety and depression, found a statistically significant positive relationship between depression scores and participants’ intent to leave (ITL) their jobs. However, the relationship between anxiety scores and ITL was not statistically significant.60
In a previous BFAS survey, conducted July–August 2021, shelters and rescue groups were asked about staffing issues. The vast majority of the 187 respondents (87%) reported staffing shortages, and 75% of organizations reported increased stress levels.b Although it is not clear if there is a direct relationship between the two, it is not unreasonable to suggest that staff shortages might lead to increased stress levels, and that increased stress levels lead to turnover (i.e. staffing shortages). Although updated figures for staffing shortages are, to our knowledge, unavailable, anecdotal information suggests that this issue persists today.
Even setting aside the animal welfare and staff well-being implications, shelter staff BO has implications for policymakers; indeed, it has been suggested that reducing BO is simply good for business.c And since roughly 76% of U.S. shelters are either operated by municipalities or private agencies with municipal contracts – accounting for approximately 80% of animals admitted to shelters annually – this is an issue likely to be of interest to taxpayers and voters.d
Work underway to mitigate the impact of job-related stress on veterinary professionals’ well-being provides some potentially useful guidance. A pilot study of veterinary professionals attending a weekly peer-support group for 10 weeks, for example, documented ‘a moderate impact on overall life stress, job satisfaction, burnout, and vicarious traumatization’. The researchers involved noted that such groups ‘may not directly impact the specific situations causing participants’ stress, but rather can impact the ability of the participant to efficiently respond to the stressor, while also offering a non-judgmental space to troubleshoot with professional peers’.e The American Animal Hospital Association’s ‘Veterinary Practice Team Well-Being’ guide offers a number of recommendations for ‘improving practice culture and team member well-being,’ ranging from the general (e.g. self-compassion and self-care) to the specific (e.g. ‘objectively assess your stress level by taking the ‘Life Stress Test’ offered by the Compassion Fatigue Awareness Project’).f Although operating a veterinary practice is not the same as operating a shelter, the many similarities offer an opportunity to learn from a field that has committed considerable resources to better understanding staff well-being in recent years.
Limitations
This study has its limitations. Any investigation using self-reported scores is prone to errors associated with inaccurate or biased responses. In the present study, we have mitigated these risks by using standard measures and a relatively large sample size. Another limitation is the study’s cross-sectional design; as a result, we are unable to definitively establish any causal ordering among the variables measured. As noted previously, shelter workers reported more depression and anxiety than those in the general population. Although it may be tempting to attribute this difference to the mentally taxing nature of shelter work, it is equally possible that a self-selection bias channels more people with symptoms of depression and anxiety into animal shelter work. In addition, the timing of our survey (i.e. when many U.S. shelters are seeing adoptions fail to keep pace with animal admissionsg) likely affected results. Repeating the survey with the same individuals at regular intervals might therefore be useful.
In addition, survey respondents were recruited largely from U.S. shelters that regularly share their data with BFAS. These shelters do not necessarily reflect U.S. shelters generally (e.g. participant shelters have higher LRRs on average, private shelters were over-represented compared to municipal shelters), which should be considered when interpreting the results of the present study.
Conclusion
Although the shelter staff we surveyed reported high levels of job satisfaction, their high BO and STS, and lower mental and physical health scores raise serious concerns about employee well-being and potential turnover following the coronavirus pandemic. If much of the trauma that comes with animal sheltering work cannot be avoided, policymakers should provide shelter staff with techniques and resources that can mitigate its impact.
Author credit statement
Peter J. Wolf: Conceptualization, methodology, data curation, and writing – original draft.
Maureen Gillespie: Conceptualization, methodology, formal analysis, and writing – review and editing.
Chris Segrin: Conceptualization, methodology, formal analysis, and writing – review and editing.
Acknowledgments
The authors would like to express our appreciation for the hundreds of shelter workers who made time in their busy, often chaotic, schedules to participate in our survey.
References
| 1. | Guerios SD, Porcher TR, Clemmer G, Denagamage T, Levy JK. COVID-19 Associated Reduction in Elective Spay-Neuter Surgeries for Dogs and Cats. Front Vet Sci. 2022;9. Accessed September 13, 2022. https://www.frontiersin.org/articles/10.3389/fvets.2022.912893 |
| 2. | Zhang S. The Great Veterinary Shortage. The Atlantic. Published online July 6, 2022. Accessed Feb 24, 2023. https://www.theatlantic.com/health/archive/2022/07/not-enough-veterinarians-animals/661497/ |
| 3. | DeSilver D. As National Eviction Ban Expires, A Look at Who Rents and Who Owns in the U.S. Pew Research Center. August 2, 2021. Accessed Apr 17, 2023. https://www.pewresearch.org/fact-tank/2021/08/02/as-national-eviction-ban-expires-a-look-at-who-rents-and-who-owns-in-the-u-s/ |
| 4. | Desilver D. Inflation Has Risen Around The World, But The U.S. Has Seen One Of The Biggest Increases. Pew Research Center. Accessed December 11, 2023. https://www.pewresearch.org/short-reads/2021/11/24/inflation-has-risen-around-the-world-but-the-u-s-has-seen-one-of-the-biggest-increases/ |
| 5. | NIH. Patient-Reported Outcomes Measurement Information System (PROMIS). National Institutes of Health; 2023. Accessed Dec 11, 2023. https://commonfund.nih.gov/promis/index |
| 6. | Bevans M, Ross A, Cella D. Patient-Reported Outcomes Measurement Information System (PROMIS): Efficient, standardized tools to measure self-reported health and quality of life. Nurs Outlook. 2014;62(5):339–345. doi: 10.1016/j.outlook.2014.05.009 |
| 7. | Broderick JE, DeWitt EM, Rothrock N, Crane PK, Forrest CB. Advances in Patient-Reported Outcomes: The NIH PROMIS® Measures. EGEMS (Wash DC). 2013;1(1):1015. doi: 10.13063/2327-9214.1015 |
| 8. | Stamm BH. The Concise ProQOL Manual. 2nd ed.; 2010. Accessed Jun 23, 2022. https://proqol.org/proqol-manual |
| 9. | Singh J, Karanika-Murray M, Baguley T, Hudson J. A Psychometric Evaluation of Professional Quality of Life Scale Version 5 (ProQOL 5) in a UK-Based Sample of Allied Mental Health Professionals. Curr Psychol. 2024;43(25):21615–21629. doi: 10.1007/s12144-024-05966-x |
| 10. | Burnett HJ. Revisiting the Compassion Fatigue, Burnout, Compassion Satisfaction, and Resilience Connection Among CISM Responders. J Police Emerg Response. 2017;7(3):1–10. doi: 10.1177/2158244017730857 |
| 11. | Geoffrion S, Lamothe J, Morizot J, Giguère CÉ. Construct Validity of the Professional Quality of Life (ProQoL) Scale in a Sample of Child Protection Workers. J Traumatic Stress. 2019;32(4):566–576. doi: 10.1002/jts.22410 |
| 12. | Watkins D. Examining the Relationship between Self-Efficacy and Quality of Life in Ocean Lifeguards. M.S. California State University, Long Beach; 2019. Accessed Jun 6, 2023. https://www.proquest.com/docview/2272840911/abstract/E59E0BEE60B24B90PQ/1 |
| 13. | Cragun JN, April MD, Thaxton RE. The Impact of Combat Deployment on Health Care Provider Burnout in a Military Emergency Department: A Cross-Sectional Professional Quality of Life Scale V Survey Study. Military Med. 2016;181(8):730–734. doi: 10.7205/MILMED-D-15-00420 |
| 14. | Lopez J, Bindler RJ, Lee J. Cross-Sectional Analysis of Burnout, Secondary Traumatic Stress, and Compassion Satisfaction Among Emergency Nurses in Southern California Working Through the COVID-19 Pandemic. J Emerg Nurs. 2022;48(4):366–375.e2. doi: 10.1016/j.jen.2022.03.008 |
| 15. | Signal T, Casey A, Taylor N. Does The Talk Match the Numbers? ProQOL and Compassion Fatigue in Animal Rescue. Traumatology. 2022;29(2):174–182. doi: 10.1037/trm0000384 |
| 16. | Rank MG, Zaparanick TL, Gentry JE. Nonhuman-Animal Care Compassion Fatigue: Training as Treatment. Best Pract Mental Health. 2009;5:40–61. |
| 17. | Andrukonis AS, Hall NJ, Hohman ZP. Group Identification and Employer Support Predict Lower Occupational Stress in Animal Shelter Employees. 2024. doi: 10.1163/15685306-bja10199 |
| 18. | Andrukonis A, Hall NJ, Protopopova A. The Impact of Caring and Killing on Physiological and Psychometric Measures of Stress in Animal Shelter Employees: A Pilot Study. Int J Environ Res Public Health. 2020;17(24). doi: 10.3390/ijerph17249196 |
| 19. | Andrukonis A, Protopopova A. Occupational Health of Animal Shelter Employees by Live Release Rate, Shelter Type, and Euthanasia-Related Decision. Anthrozoös. 2020;33(1):119–131. doi: 10.1080/08927936.2020.1694316 |
| 20. | Rohlf V, Bennett P. Perpetration-Induced Traumatic Stress in Persons Who Euthanize Nonhuman Animals in Surgeries, Animal Shelters, and Laboratories. Soc Anim. 2005;13(3):201–219. |
| 21. | Validation. Accessed Nov 29, 2023. https://www.healthmeasures.net/explore-measurement-systems/promis/measure-development-research/validation |
| 22. | Stamm BH. The ProQOL Manual. 2005. |
| 23. | Figley CR, ed. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized. Taylor & Francis Group, LLC; 1995. |
| 24. | Abendroth M, Flannery J. Predicting the Risk of Compassion Fatigue: A Study of Hospice Nurses. J Hosp Palliat Nurs. 2006;8(6):346. |
| 25. | McMullen L. Oncology Nursing and Compassion Fatigue: Caring Until It Hurts. Who Is Caring for the Caregiver? Oncol Nurs Forum. 2007;34(2):491–492. |
| 26. | Eastwood CD, Ecklund K. Compassion Fatigue Risk and Self-Care Practices Among Residential Treatment Center Childcare Workers. Residential Treat Child Youth. 2008;25(2):103–122. doi: 10.1080/08865710802309972 |
| 27. | Smith N. A Questionnaire Based Study to Assess Compassion Fatigue in UK Practising Veterinary Nurses. Vet Nurs. 2016;7(7):418–425. doi: 10.12968/vetn.2016.7.7.418 |
| 28. | Scotney RL. Occupational Stress & Compassion Fatigue: The Effects on Workers in Animal-Related Occupations. PhD Thesis. The University of Queensland; 2017. doi: 10.14264/uql.2017.502 |
| 29. | Scotney RL, Deidre McLaughlin, Helen L Keates. An Investigation of the Prevalence of Compassion Fatigue, Compassion Satisfaction and Burnout in Those Working in Animal-Related Occupations using the Professional Quality of Life (ProQoL) Scale. Vet Nurs. 2019;10(5):276–284. |
| 30. | Rogelberg SG, Reeve CL, Spitzmüller C, et al. Impact of Euthanasia Rates, Euthanasia Practices, and Human Resource Practices on Employee Turnover in Animal Shelters. J Am Vet Med Assoc. 2007;230(5):713–719. doi: 10.2460/javma.230.5.713 |
| 31. | Scotney RL, McLaughlin D, Keates HL. A Systematic Review of the Effects of Euthanasia and Occupational Stress in Personnel Working with Animals in Animal Shelters, Veterinary Clinics, and Biomedical Research Facilities. J Am Vet Med Assoc. 2015;247(10):1121–1130. doi: 10.2460/javma.247.10.1121 |
| 32. | Baran BE, Rogelberg SG, Carello Lopina E, Allen JA, Spitzmüller C, Bergman M. Shouldering a Silent Burden: The Toll of Dirty Tasks. Hum Relat. 2012;65(5):597–626. doi: 10.1177/0018726712438063 |
| 33. | Monaghan H, Rohlf V, Scotney R, Bennett P. Compassion Fatigue in People Who Care for Animals: An Investigation of Risk and Protective Factors. Traumatology. 2020;30(1):77–85. doi: 10.1037/trm0000246 |
| 34. | n.a. HealthMeasures: Scoring Instructions. HealthMeasures (Northwestern University). 2023. Accessed Oct 23, 2023. https://www.healthmeasures.net/score-and-interpret/calculate-scores/scoring-instructions |
| 35. | Samios C, Rodzik AK, Abel LM. Secondary Traumatic Stress and Adjustment in Therapists Who Work with Sexual Violence Survivors: The Moderating Role of Posttraumatic Growth. Br J Guidance Counsell. 2012;40(4):341–356. doi: 10.1080/03069885.2012.691463 |
| 36. | de Goeij MCM, van Diepen M, Jager KJ, Tripepi G, Zoccali C, Dekker FW. Multiple Imputation: Dealing with Missing Data. Nephrol Dialysis Transpl. 2013;28(10):2415–2420. doi: 10.1093/ndt/gft221 |
| 37. | De La Rosa GM, Webb-Murphy JA, Fesperman SF, Johnston SL. Professional Quality of Life Normative Benchmarks. Psychol Trauma. 2018;10:225–228. doi: 10.1037/tra0000263 |
| 38. | ASPCA. What is Your Rate? Understanding the Asilomar Live Release Rate, ASPCA Live Release Rate and Save Rate. 2011. Accessed Jan 14, 2018. http://www.aspcapro.org/sites/pro/files/What%20is%20your%20Rate%2010_2013.pdf |
| 39. | Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J Royal Statistical Society: Series B (Methodological). 1995;57(1): 289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x |
| 40. | Sharma A, Minh Duc NT, Luu Lam Thang T, et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J Gen Intern Med. 2021;36(10):3179–3187. doi: 10.1007/s11606-021-06737-1 |
| 41. | n.a. Labor Force Statistics from the Current Population Survey. U.S. Bureau of Labor Statistics; 2024. Accessed Jun 11, 2024. https://www.bls.gov/cps/cpsaat11.htm |
| 42. | Busse M, Stromgren K, Thorngate L, Thomas KA. Parent Responses to Stress: PROMIS in the NICU. Crit Care Nurse. 2013;33(4):52–60. doi: 10.4037/ccn2013715 |
| 43. | Imes CC, Chasens ER. Rotating Shifts Negatively Impacts Health and Wellness Among Intensive Care Nurses. Workplace Health Saf. 2019;67(5):241–249. doi: 10.1177/2165079918820866 |
| 44. | Christopher MS, Hunsinger M, Goerling RJ, et al. Mindfulness-Based Resilience Training to Reduce Health Risk, Stress Reactivity, and Aggression among Law Enforcement Officers: A Feasibility and Preliminary Efficacy Trial. Psychiatry Res. 2018;264:104–115. doi: 10.1016/j.psychres.2018.03.059 |
| 45. | Thurston SE, Chan G, Burlingame LA, Jones JA, Lester PA, Martin TL. Compassion Fatigue in Laboratory Animal Personnel during the COVID-19 Pandemic. J Am Assoc Lab Anim Sci. 2021;60(6):646. doi: 10.30802/AALAS-JAALAS-21-000030 |
| 46. | Davies LE, Brooks M, Braithwaite EC. Compassion Fatigue, Compassion Satisfaction, and Burnout, and Their Associations with Anxiety and Depression in UK Police Officers: A Mixed Method Analysis. Pol J. 2022:0032258X221106107. doi: 10.1177/0032258X221106107 |
| 47. | Hannah B, Woolgar M. Secondary Trauma and Compassion Fatigue in Foster Carers. Clin Child Psychol Psychiatry. 2018;23(4):503–662. doi: 10.1177/1359104518778327 |
| 48. | Rohlf VI, Scotney R, Monaghan H, Bennett P. Predictors of Professional Quality of Life in Veterinary Professionals. J Vet Med Educ. 2022;49(3);372–386. doi: 10.3138/jvme-2020-0144 |
| 49. | Knight MD. The Quality of Life in Mental Health Professionals Treating Military Service Members with Combat Trauma. Ph.D. Northcentral University; 2022. Accessed Jun 2, 2023. https://www.proquest.com/docview/2803147102/abstract/26AE7DA03A6F4A35PQ/1 |
| 50. | Powell T, Billiot S, Muller J, Elzey K, Brandon A. The Cost of Caring: Psychological Adjustment of Health-Care Volunteers During the COVID-19 Pandemic. Traumatology. 2022;28(3):383–392. doi: 10.1037/trm0000387 |
| 51. | Cunningham T, Catallozzi M, Rosenthal D. Camaraderie and Community: Buffers against Compassion Fatigue among Expatriate Healthcare Workers during the Ebola Epidemic of 2013–16. Health Emerg Disaster Nurs. 2018;5(1):2–11. doi: 10.24298/hedn.2016-0014 |
| 52. | Daily TA. Fostering Rescued Dogs: An Exploratory Study of the Experiences of Foster Care Providers. Human-Anim Interact Bull. 2021;2021. doi: 10.1079/hai.2021.0008 |
| 53. | Copeland D, Henry M. The relationship between workplace violence, perceptions of safety, and Professional Quality of Life among emergency department staff members in a Level 1 Trauma Centre. Int Emerg Nurs. 2018;39:26–32. doi: 10.1016/j.ienj.2018.01.006 |
| 54. | Staudt M, Williams-Hayes M. Secondary Traumatic Stress, Burnout, and Compassion Satisfaction Among Child Advocacy Interdisciplinary Team Members. ASW. 2020;19(2):416–429. doi: 10.18060/22957 |
| 55. | Salimi S, Pakpour V, Rahmani A, Wilson M, Feizollahzadeh H. Compassion Satisfaction, Burnout, and Secondary Traumatic Stress Among Critical Care Nurses in Iran. J Transcult Nurs. 2020;31(1):59–66. doi: 10.1177/1043659619838876 |
| 56. | Seemann NM, Karanicolas PJ, Guttman MP, et al. Compassion Fatigue in Surgical Trainees. J Surg Educ. 2019;76(5):1211–1222. doi: 10.1016/j.jsurg.2019.03.012 |
| 57. | Bredehorst J, Krautter K, Meuris J, Jachimowicz JM. The Challenge of Maintaining Passion for Work over Time: A Daily Perspective on Passion and Emotional Exhaustion. Org Sci. 2023;35(1);364–386. doi: 10.1287/orsc.2023.1673 |
| 58. | Aminihajibashi S, Skar AMS, Jensen TK. Professional Wellbeing and Turnover Intention among Child Therapists: A Comparison between Therapists Trained and Untrained in Trauma-Focused Cognitive Behavioral Therapy. BMC Health Serv Res. 2022;22(1):1328. doi: 10.1186/s12913-022-08670-3 |
| 59. | Wells-English D, Giese J, Price J. Compassion Fatigue and Satisfaction: Influence on Turnover Among Oncology Nurses at an Urban Cancer Center. Clin J Oncol Nurs. 2019;23(5):487–493. doi: 10.1188/19.CJON.487-493 |
| 60. | Ligibel JA, Goularte N, Berliner JI, et al. Well-Being Parameters and Intention to Leave Current Institution Among Academic Physicians. JAMA Netw Open. 2023;6(12):e2347894. doi: 10.1001/jamanetworkopen.2023.47894 |
| 61. | Storozuk A, Ashley M, Delage V, Maloney EA. Got Bots? Practical Recommendations to Protect Online Survey Data from Bot Attacks. TQMP. 2020;16(5):472–481. doi: 10.20982/tqmp.16.5.p472 |
| 62. | Griffin M, Martino RJ, LoSchiavo C, et al. Ensuring Survey Research Data Integrity in the Era of Internet Bots. Qual Quant. 2022;56(4):2841–2852. doi: 10.1007/s11135-021-01252-1 |
| 63. | Zhang Z, Zhu S, Mink J, Xiong A, Song L, Wang G. Beyond Bot Detection: Combating Fraudulent Online Survey Takers. In: Proceedings of the ACM Web Conference 2022. ACM; 2022: 699–709. doi: 10.1145/3485447.3512230 |
Appendix A: Data cleaning details
Detecting the bot attacks was relatively straightforward since the response rate was observed to increase dramatically (i.e. 320 surveys begun within a 30-min period). Identifying the valid responses was more difficult, however. In some cases, there were obvious signs of trouble, such as submissions having internet protocol (IP) addresses outside the U.S. or with dubious shelter names (e.g. ‘Virginia Zoo’, ‘pound’, or ‘puppy’). Hundreds of submissions appeared to legitimate, however, with valid shelter names, IP addresses, etc.
An invalid shelter name (determined by checking against a list of U.S. shelters that is maintained by BFAS) was reason enough to reject a submission. Following the advice of other researchers,61–63 we developed a screening system comprised of multiple flags (e.g. Qualtrics reCAPTCHA score < 0.5 or fraud detection score ≥ 30, suspect IP location, etc.). A minimum of 2 flags were required to reject a submission. However, flags were not necessarily valued equally. A mismatch between IP location and shelter location, for example, was not sufficient cause to reject a submission. It might be the case, for example, that a staff member was working off-site when they completed our survey or accessed the survey via a virtual private network (VPN), thereby masking their true location. Another ‘false positive’ we sometimes observed was the flag generated by Qualtrics when the system detects multiple submissions from the same IP address. We could determine that, in some cases, multiple staff members were using the same device to complete our survey, often one after another. E-mail addresses were rarely of much help, as we encouraged participants to use their personal e-mail address rather than one associated with their employer. However, the few submissions for which we had verifiable e-mail addresses proved invaluable for validating our system of flags (e.g. confirming that a dubious IP location alone was not evidence of a fraudulent submission).
Footnotes
a. BFAS. The State of U.S. Animal Sheltering, 2022. Best Friends Animal Society; 2023:5. Accessed October 24, 2023. https://network.bestfriends.org/sites/default/files/2023-06/National%20Shelter%20Data%20Set%202023_updated_6.12.2023.pdf
b. BFAS. Staffing Shortage Survey Data. Best Friends Animal Society; 2021. Accessed February 24, 2023. https://network.bestfriends.org/research-data/research/staffing-shortage-survey-data
c. Sears L, Nelms D, Mahan TF. 2017 Retention Report. Work Institute; 2017:31. Accessed September 25, 2023. https://info.workinstitute.com/retentionreport2017; Otto N. Avoidable turnover costing employers big. Employee Benefit News. Published August 9, 2017. Accessed July 27, 2023. https://www.benefitnews.com/news/avoidable-turnover-costing-employers-big.
d. Based on data compiled by BFAS.
e. Kieschnick D, Lawlor K. Veterinary Mental Health Initiative Pilot Program Results. Shanti Project; 2021.
f. Cavanaugh MT, Gaspar M, Hall R, et al. AAHA’s Guide to Veterinary Practice Team Wellbeing. American Animal Hospital Association; 2019:18. https://www.aaha.org/globalassets/04-practice-resources/practice-culture/team_wellbeing_guide.pdf
g. BFAS. The State of U.S. Animal Sheltering, 2022. Best Friends Animal Society; 2023:5. Accessed October 24, 2023. https://network.bestfriends.org/sites/default/files/2023-06/National%20Shelter%20Data%20Set%202023_updated_6.12.2023.pdf