ORIGINAL RESEARCH ARTICLE
Success of outpatient treatment for canine parvovirus in a subsidized community medicine clinic in Florida
Veronica H. Accornero1*, Carolyn Brown2, Margaret R. Slater1, Christina Hawkins2 and Molly Sumridge1
1Strategy and Research, American Society for the Prevention of Cruelty to Animals, New York, NY, USA; 2Community Medicine, American Society for the Prevention of Cruelty to Animals, New York, NY, USA
Abstract
Introduction: Typical inpatient treatment for canine parvovirus (CPV) is expensive and unaffordable for many pet owners. Outpatient treatment may be a viable alternative when hospitalization is inaccessible due to finances or other barriers. This study aimed to determine survival for dogs receiving a once-daily clinic visit outpatient treatment protocol for CPV in a community medicine clinic. Potential predictors of survival, as well as owner-reported treatment satisfaction and feasibility, were also examined.
Methods: Within a prospective, observational design, data including patient history, clinical signs, treatments received, and treatment outcome were captured in the medical record. Owners were invited to complete a survey about their treatment experience. Survival and survey responses were summarized using counts and percentages. Logistic regression modeling was used to evaluate potential predictors of survival.
Results: During the study period of October 1, 2021, to September 30, 2023, 113 dogs met the inclusion criteria and were treated with the once-daily outpatient CPV protocol. Of these, 73 survived, 23 died, two were euthanized during treatment, and 15 were lost to follow-up. Seventy-four percent (73/98, 95% confidence interval, 65%–83%) of those with a known outcome survived. Requiring and receiving ≥ 2 days of subcutaneous fluids, having pale mucous membranes at baseline, and being referred for and receiving weekend treatment at a partner clinic predicted decreased survival, while having ≥ 3 total once-daily clinic visits was associated with increased survival. Most owners reported that the treatments were easy to administer and that they had a positive experience and were satisfied with the treatment.
Conclusion: Findings build upon existing research showing good outcomes with lower-cost CPV treatment, adding another evidence-based option to tailor treatment to the needs and preferences of the patient, client, clinic, and community. Offering outpatient treatment within a spectrum of care approach can increase access to care for more dogs with parvovirus.
Keywords: dogs; survival; access to care; lower cost; spectrum of care; client perspective
Citation: Journal of Shelter Medicine and Community Animal Health 2025, 4: 131 - http://dx.doi.org/10.56771/jsmcah.v4.131
Copyright: © 2025 Veronica H. Accornero et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 25 March 2025; Revised: 28 July 2025; Accepted: 30 July 2025; Published: 21 October 2025
Competing interests and funding: No external funding was used in this study. The authors declare that there were no conflicts of interest.
Correspondence: *Veronica H. Accornero, Director, Department of Strategy and Research, American Society for the Prevention of Cruelty to Animals, New York, NY, USA. Email: veronica.accornero@aspca.org
Reviewers: Paulo Afonso
Hayley Hadden
Veterinary care supports the health and well-being of animals, families, and communities, yet millions of animals lack this necessary care.1 According to a 2018 national survey of pet owners, approximately 28% indicated that they were unable to access needed veterinary care for their pets during the last 2 years. This was particularly true for preventative care such as vaccines and medical exams, which are critical for the prevention of communicable diseases and early detection and treatment of other conditions.2
Canine parvovirus (CPV) is a highly contagious virus that is common in puppies and young dogs, with mortality rates as high as 91% without treatment.3,4 Although a vaccine exists, CPV is still prevalent in general and emergency practices, potentially due in part to inadequate access to preventive veterinary care. Treatment for CPV is considered supportive and typically consists of intravenous fluids, electrolyte supplementation, antibiotics, antiemetics, antacids, and analgesics with continuous monitoring in a 24-h care setting.4,5 Treatment is effective in many cases, but also very expensive and unaffordable for many pet owners.4,6,7 When typical 24-h hospitalization or alternative care is not available due to financial limitations or other barriers, euthanasia may be considered as the only advisable alternative. As a result, a diagnosis of CPV can lead to distress and difficult decisions for pet owners and veterinarians alike.
The most commonly reported barrier to accessing care is financial.2,8,9 Access to veterinary care is a concern for families at all income levels.2 King et al.10 found that financial fragility (the ability to come up with $2,000 for an unexpected need within the next month) was prevalent across all income brackets under $200,000 per year, indicating that even middle- and upper-income families may struggle to pay for emergency or specialized veterinary treatment. Other challenges to accessing veterinary care include a lack of transportation, limited clinic hours, language barriers, and unsatisfactory previous experiences with veterinary and medical professionals.2,11,12
Outpatient parvovirus treatment, costing hundreds of dollars compared to thousands for inpatient care, may be a viable alternative.13 Typically, outpatient treatment involves daily examinations, subcutaneous fluids, and medications in the clinic, along with additional at-home treatments and/or monitoring.13–15 A few studies have examined outpatient treatment of CPV and shown it to be much better than no treatment, with outcomes comparable to inpatient treatment. In the first study to evaluate a standardized protocol for outpatient treatment, Venn et al.14 randomized dogs to either inpatient (n = 20) or outpatient (n = 20) treatment and reported survival rates of 90% (95% CI [confidence interval], 68–99%) and 80% (95% CI, 56–94%), respectively, which were not statistically different (p = 0.66). Although the outpatient protocol14 (the Colorado State University Protocol) was meant to parallel home treatment, dogs in both groups remained hospitalized for close monitoring and to ensure treatment compliance. Therefore, whether study results can be generalized to an actual outpatient setting is unclear.
In another study, Sarpong et al.15 retrospectively reviewed medical records from a private veterinary clinic serving low-income owners. They found that 75% (95% CI, 66–82%) of dogs (n = 130) treated for CPV as outpatients survived. A standardized treatment protocol was not followed, so it is unclear how to translate the approach to other clinics. Most recently, Perley et al.13 adapted the Colorado State protocol for a shelter-based, low-cost clinic, where treatments were administered during morning and afternoon visits to the clinic and with at-home monitoring overnight. Eighty-three percent (95% CI, 74–90%) of dogs (n = 95) treated with the protocol survived. That study demonstrated that standardized outpatient treatment could be implemented at substantially reduced cost (i.e. $479 vs. an estimated $3,000–5,000 for inpatient care) and with reasonable outcomes in a low-cost clinic. However, the Perley protocol required twice-daily clinic visits and included bloodwork and rescue IV fluids, which may not be feasible for some clients and clinics. Additionally, none of the CPV outpatient studies assessed the client’s experience with treatment. This is particularly important with outpatient CPV protocols, given the increased responsibility for clients (e.g., frequent clinic visits and at-home treatments). Also, implementation in underserved communities, where clients often face barriers to care, may impact treatment adherence and outcomes.
Given the limitations of previous studies, further research is necessary to evaluate simplified protocols in real-world outpatient settings, especially in underserved areas. This current study aimed to evaluate the success and feasibility of a less intensive outpatient treatment protocol, which required once-daily clinic visits and no additional diagnostics beyond a SNAP® Parvo Test, implemented as standard clinical practice in a community medicine clinic located in an underserved urban neighborhood in Florida. The primary objective was to determine survival for dogs treated using the protocol and to compare it with other published outpatient and inpatient treatment studies. The study also sought to identify potential predictors of survival and to understand client experience. The hypothesis was that survival rates would be comparable to those in other outpatient studies and that most clients would find the treatment acceptable and manageable.
Methods
Study design
This was a prospective, observational study of dogs diagnosed with CPV and treated with the once-daily outpatient treatment protocol at The American Society for the Prevention of Cruelty to Animals® Miami Community Veterinary Clinic (CVC) between October 1, 2021, and September 30, 2023. The clinic provides free and low-cost services to pets and their owners in a community where veterinary options, including preventive care, are limited, and many pets are unvaccinated. Inclusion criteria: (1) presentation with clinical signs consistent with CPV (i.e., sudden onset of vomiting, diarrhea, inappetence, and/or lethargy) and (2) a positive IDEXX SNAP® Parvo Test (IDEXX Laboratories, Westbrook, Maine) via rectal swab. Exclusion criteria: (1) not having IDEXX SNAP® Parvo Test result on file; (2) a negative parvovirus test; (3) receiving treatment inconsistent with the protocol (i.e., overnight hospitalization and/or receipt of intravenous fluids) at another facility; or (4) exhibiting severe signs such as recumbency, non-response, and/or shock.
Medical data were captured in the electronic medical record and extracted at the end of the study. Records were monitored periodically for completeness and accuracy; additional staff training was provided as needed. To assess client experience, owners were invited to participate in a voluntary, short survey about the treatment process. The American Society for the Prevention of Cruelty to Animals® Committee on Animals as Research Participants and Ethics provided ethical approval for animal participation in this study (Protocol #7-29-2024-Outpatient Parvo), and Solutions Institutional Review Board provided ethical approval for human participation (Protocol # 2021/02/31).
Treatment protocol
Patients presented at the CVC by appointment or on a walk-in basis. Dogs suspected of CPV were met outside and administered an in-house rectal swab SNAP® test for CPV. Patients testing positive or strongly suspected of CPV were carried directly to the treatment room, minimizing contacts. Following the exam, the veterinarian explained CPV and discussed treatment options with the owner. Referral for inpatient, specialized care was recommended for all patients. If the owner indicated that this was not feasible due to financial limitations or other barriers, the outpatient protocol, which is standard of care at the CVC, was described, and the risks and benefits were discussed. The owner consented to treatment by signing a standardized clinic consent form at each visit. All services, including the SNAP® Parvo Test, exams, and clinic and at-home treatments, were provided at no charge to the owner.
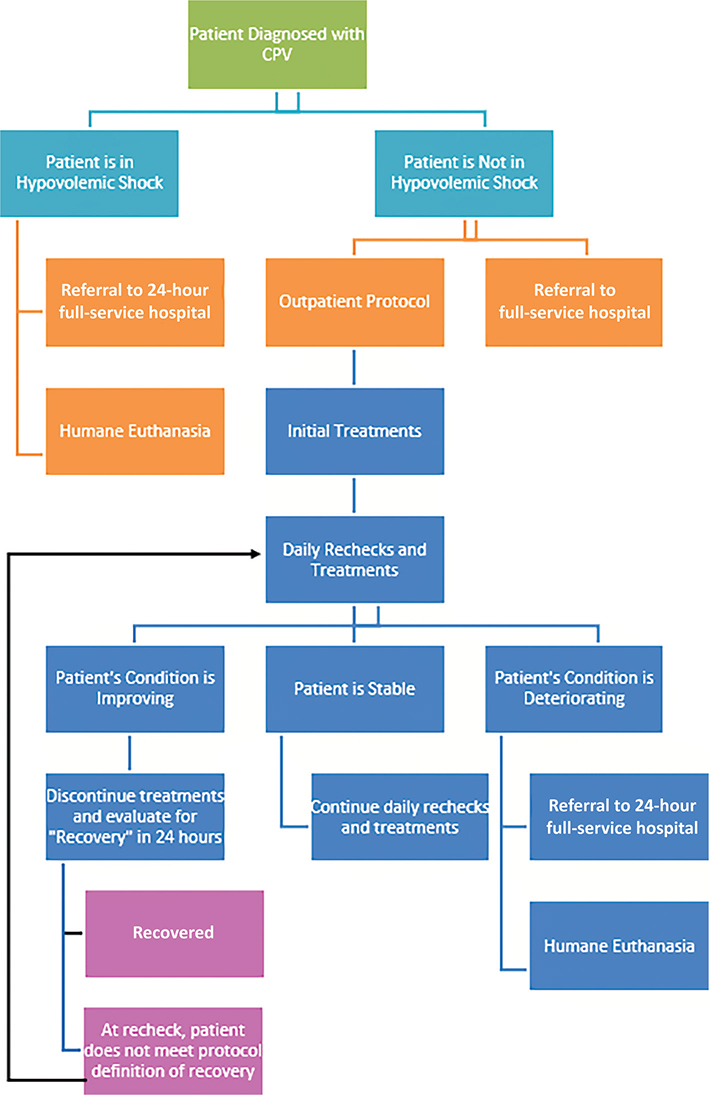
Outpatient treatment is generally indicated for patients who are stable. Patients presenting with severe symptoms were referred for inpatient treatment or offered euthanasia as appropriate. However, most clients presenting to the clinic could not afford inpatient care and did not have other options for care. Unless the patient was so ill that euthanasia was the most humane option or was elected by the owner due to other considerations, outpatient care was offered in most cases.
Participants received treatment according to the CVC’s CPV Outpatient Treatment Protocol (Appendix 1), which simplifies the protocol published by Perley et al.13 by eliminating bloodwork and rescue intravenous fluids and reducing clinic visits to once daily (typically in the morning) for examination and treatments. All treating veterinarians were full-time employees of the clinic and were trained on and followed the outpatient treatment protocol. Differences in clinical judgement among attending veterinarians were mitigated through case discussions and the sharing of patient responsibilities. Owners were instructed on how to administer subcutaneous (SQ) fluids at home and provided with the necessary supplies for evening treatment, as clinically indicated. If treatment was needed on days when the CVC was closed, arrangements were made at a private partner clinic that agreed to follow the outpatient protocol (at the expense of the CVC). If owners could not visit the partner clinic, medications and fluids were dispensed for at-home treatments when possible. All staff members used personal protective equipment, including disposable gowns, gloves, and shoe covers, during interactions with the patient. Following treatment, patients were carried directly out of the clinic. All treatment room surfaces were disinfected with Rescue® for 5 min at a 1:16 concentration, and floors were disinfected with bleach at a 1:32 dilution.
Medical record review
Medical records were reviewed for dogs with a possible diagnosis of CPV between October 1, 2021, and September 30, 2023. Data were extracted directly from fields in the electronic medical record when possible. Additional variables manually coded after reviewing all information in the medical record were duration of clinical signs, prior treatment (by the owner or other veterinarian), vomiting, diarrhea, decreased eating, decreased drinking, vaccination status, number of visits to the clinic, number of days received fluids in the clinic, and whether fluids were administered at home. Dogs were considered vaccinated if they had received at least one round of the distemper, hepatitis, parvovirus, parainfluenza (DHPP) vaccine more than 3 days prior to diagnosis. If the vaccine was administered at the CVC, it was a modified live vaccine. If the vaccine was administered at another clinic, this was reported by the owner, and medical records were typically unavailable to verify the vaccine types. For dogs referred to a partner clinic, their records were coded to indicate the number of visits and treatments received, including any treatments inconsistent with the outpatient protocol (e.g., overnight hospitalization, IV fluids, etc.) that might warrant exclusion from the study. Protocol outcome, coded as survived, died, euthanized, or lost to follow-up (LTF), was determined through a review of the medical record. In cases where the outcome was unclear in the medical record, clinic staff attempted to contact owners via phone to determine the outcome. Cases were considered LTF after three unsuccessful attempts to reach owners for status via text and telephone.
Client survey
At the last treatment visit, owners were invited to participate in a brief, voluntary survey regarding their experience with the CPV outpatient treatment (Appendix 2). The survey was offered in English and Spanish. Verbal consent was obtained prior to beginning the survey. The survey was self-administered or staff-administered, depending on the owner’s preference, via SurveyMonkey and iPad. Timing of survey was in person at the last visit or over the phone, ideally within 2–3 weeks if the owner was unable to complete the survey at the last visit or did not return for a final visit. Owners with more than one dog receiving outpatient treatment were invited to complete a survey for each dog.
Statistical analysis
All analyses were conducted using Stata.16 Categorical variables were described using counts and percentages, and continuous variables were summarized using medians and minimum/maximum. The primary outcome variable was survival (yes/no), summarized with a 95% CI. To identify potential prognostic indicators, bivariate analyses of survival with each of the following categorical variables (coded yes/no except where indicated) were performed using Fisher’s exact tests: breed (Terrier types, Bulldog types, Shepherds and mixes, Chihuahuas and mixes, Boxers, Shih Tzu, unspecified mixes, other breeds), sex (female/male), intact status, prior vaccines, prior treatment, vomiting, diarrhea, decreased eating, decreased drinking, body condition score (BCS; 1, 2, 3, 4, 5), hydration status (normal, 5% dehydrated, 10% dehydrated), mucous membrane hydration (moist, tacky), mucous membrane color (pale, pink), capillary refill time (CRT; < 2 s, ≥ 2 s), mentation [Bright, Alert, and Responsive (BAR); Quiet, Alert, and Responsive (QAR); Depressed], intestinal parasites, days treated at partner clinics (0, 1, 2, 3 days), days receiving fluids at partner clinics (0, 1, 2, 3 days), prescribed Nutrical, and at-home fluids. Breed was collapsed based on general types/mixes where there were four or more of that group; other breeds were then combined into a single category for analysis. The number of treatment days at partner clinics and the number of days receiving fluids at partner clinics were considered categorical, as the maximum duration was 3 days. Wilcoxon rank-sum tests were used for each continuous variable: baseline age (months), weight (kg), temperature (°F), days with clinical signs before presentation, number of treatment days at the CVC, total number of treatment days (sum of the number of treatment days at CVC and partner clinic), number of days receiving fluids at the CVC, and total number of days receiving fluids (sum of fluid days at CVC and partner clinic). Missing data were excluded from analyses. LTF cases were removed for analyses of survival.
Logistic regression models used backwards stepwise selection and the likelihood ratio test to identify the most parsimonious base model. Variables with p ≤ 0.25 in the bivariate analyses were included in preliminary modeling as potential predictors (base model). After backwards selection (p < 0.05), each variable omitted was then offered to the base model and tested via the likelihood ratio test again. If multiple variables were significant when added to the base model, the model with the greatest area under the curve was kept. Collinearity or zero cells among independent variables were identified in the stepwise process by variables or observations being omitted by the software. Those variables were collapsed when feasible. If recoding was not an option, they were removed from the initial backwards stepwise process one at a time until no observations were omitted due to estimability. Relevant interaction terms were tested for statistical significance; if significant, they became part of the final model. Odds ratios, their 95% CIs, Hosmer–Lemeshow goodness-of-fit test, and area under the receiver operating characteristic curve (AUC) were calculated for the final model.
Owner survey responses were described using counts and percentages. For five-point Likert questions, responses were collapsed into three categories, combining the two lower-end categories (‘not at all/slightly’) and the two upper-end categories (‘mostly/completely’). The survey included six open-ended questions intended to elicit qualitative insights from owners. However, five of the six questions received two or fewer responses and were excluded from thematic analysis due to insufficient data. The remaining question, ‘Anything more you would like to tell us about your answers above or your experience with the treatment for this illness (canine parvovirus) in your dog?’ received 25 responses and was subsequently analyzed for themes and sentiment. Responses were reviewed inductively to identify recurring themes and sentiment related to owners’ experiences with their dog’s CPV treatment.
Results
A total of 163 dogs with presumptive or confirmed diagnoses for CPV were seen at the CVC during the 2-year study. Fifty dogs were excluded from the study due to a negative parvovirus test (n = 28), no parvovirus test result in the medical record (n = 11), care inconsistent with the protocol at the partner clinics (n = 5), euthanasia before treatment (n = 4), and owners sought treatment elsewhere after diagnosis (n = 2). Dogs who were euthanized presented with clinical signs such as severe dehydration, depressed mentation, minimal/non-responsiveness, and/or lateral presentation; after discussing the prognosis with the owners, the owners elected euthanasia as the best option. The resulting sample for the study was 113 dogs from 94 owners.
The sample had a median age of 3.7 months (range: 1–60 months). Seventeen breeds or mixes were represented (Table 1). Of those with known vaccination status, only 29% (23/79) had at least one round of the DHPP vaccine. The duration of clinical signs before presentation to the clinic ranged from 1 to 14 days (median = 2 days); one dog was reported to have had clinical signs for 14 days and was a potential false-positive result.
| Variable | Non-survivors n = 25 No. (%) |
Survivors n = 73 No. (%) |
P-value |
| Characteristic | |||
| Age (months)a | 3.1 (1.8–12) | 3.0 (1.0–60) | 0.7 |
| Sexb | 0.2 | ||
| Female | 7 (18) | 32 (82) | |
| Male | 18 (31) | 41 (69) | |
| Intact | – | ||
| No | 0 (0) | 0 (0) | |
| Yes | 25 (26) | 73 (74) | |
| Breedc | 0.6 | ||
| Terrier types | 9 (27) | 24 (73) | |
| Unspecified mixes | 4 (24) | 13 (76) | |
| Other breeds | 3 (19) | 13 (81) | |
| Bulldog types | 7 (47) | 8 (53) | |
| Shepherds and mixes | 1 (20) | 4 (80) | |
| Chihuahuas and mixes | 0 (0) | 4 (100) | |
| Boxers | 0 (0) | 4 (100) | |
| Shih Tzu | 1 (25) | 3 (75) | |
| Patient history | |||
| Prior vaccines | 1.0 | ||
| No | 14 (29) | 34 (71) | |
| Yes | 5 (28) | 13 (72) | |
| Missing | 6 (19) | 26 (81) | |
| Clinical signs duration (days)a | 2 (1–7) | 3 (1–7) | 0.6 |
| Missing | 8 (36) | 14 (64) | |
| Prior treatment | 0.4 | ||
| No | 24 (27) | 65 (73) | |
| Yes | 1 (11) | 8 (89) | |
| Decreased eating | 1.0 | ||
| No | 2 (22) | 7 (78) | |
| Yes | 17 (22) | 62 (78) | |
| Missing | 6 (60) | 4 (40) | |
| Decreased drinking | 0.6 | ||
| No | 5 (18) | 23 (82) | |
| Yes | 14 (24) | 44 (76) | |
| Missing | 6 (50) | 6 (50) | |
| Vomiting | 1.0 | ||
| No | 2 (18) | 9 (82) | |
| Yes | 18 (23) | 59 (77) | |
| Missing | 5 (50) | 5 (50) | |
| Diarrhea | 0.7 | ||
| No | 2 (13) | 13 (87) | |
| Yes | 16 (22) | 57 (78) | |
| Missing | 7 (70) | 3 (30) | |
| Clinical signs | |||
| Temperature (°F)a | 101.7 (98.6–104.5) | 101.4 (97.9–106.0) | 0.8 |
| Missing | 1 (8) | 11 (92) | |
| Weight (kg)a | 6.9 (0.9–27) | 6.4 (1.4–27) | 0.9 |
| BCSb | 0.2 | ||
| 1 | 1 (100) | 0 (0) | |
| 2 | 2 (33) | 4 (67) | |
| 3 | 6 (21) | 22 (79) | |
| 4 | 3 (14) | 18 (86) | |
| 5 | 13 (32) | 28 (68) | |
| Missing | 0 (0) | 1 (100) | |
| Hydration | 0.9 | ||
| Normal | 10 (27) | 27 (73) | |
| 5% dehydrated | 13 (25) | 38 (75) | |
| 10% dehydrated | 2 (33) | 4 (67) | |
| Missing | 0 (0) | 4 (100) | |
| Mucous membrane hydration | 0.8 | ||
| Moist | 13 (28) | 34 (72) | |
| Tacky | 11 (24) | 35 (76) | |
| Missing | 1 (20) | 4 (80) | |
| Mucous membrane colorb | 0.1 | ||
| Pale | 3 (50) | 3 (50) | |
| Pink | 19 (22) | 68 (78) | |
| Missing | 3 (60) | 2 (40) | |
| CRT | 0.6 | ||
| < 2 s | 21 (23) | 69 (77) | |
| ≥ 2 s | 1 (33) | 2 (67) | |
| Missing | 3 (60) | 2(40) | |
| Mentation | 0.5 | ||
| BAR | 5 (26) | 14 (74) | |
| QAR | 10 (20) | 39 (80) | |
| Depressed | 9 (32) | 19 (68) | |
| Missing | 1 (50) | 1 (50) | |
| Intestinal parasites | 0.4 | ||
| No | 22 (28) | 57 (72) | |
| Yes | 3 (16) | 16 (84) | |
| Treatment | |||
| Visits- total (days)a,b | 3 (1–7) | 4 (1–10) | 0.006 |
| Visits- CVC (days)a,b | 2 (1–6) | 3 (1–9) | < 0.001 |
| Visits- partner clinicb | 0.2 | ||
| Zero | 13 (23) | 43 (77) | |
| 1 day | 8 (44) | 10 (56) | |
| 2 days | 3 (17) | 15 (83) | |
| 3 days | 1 (17) | 5 (83) | |
| Fluids- total (days)a,b | 2 (0–5) | 3 (1–8) | 0.1 |
| Missing | 1 (33) | 2 (64) | |
| Fluids- CVC (days)a,b | 2 (0–4) | 2 (1–7) | 0.1 |
| Missing | 1 (33) | 2 (64) | |
| Fluids- partner clinic | 0.3 | ||
| Zero | 16 (25) | 47 (75) | |
| 1 day | 6 (43) | 8 (57) | |
| 2 days | 2 (13) | 13 (87) | |
| 3 days | 1 (17) | 5 (83) | |
| Fluids-at homeb | 0.2 | ||
| No | 9 (33) | 18 (67) | |
| Yes | 9 (17) | 43 (83) | |
| Missing | 7 (37) | 12 (63) | |
| Nutrical prescribed | 0.8 | ||
| No | 18 (27) | 49 (73) | |
| Yes | 7 (23) | 24 (77) | |
| CRT: capillary refill time; BAR: Bright, Alert, and Responsive; QAR: Quiet, Alert, and Responsive; CVC: Community Veterinary Clinic. aMedian (range); bVariables entered in multivariable logistic regression modeling; cOther breeds included 3 each mastiffs and mixes, Malteses, rottweilers and Yorkshire terriers, 2 Pomeranians, and 1 each dachshund, Siberian husky, Labrador retriever, and toy poodle. |
|||
Dogs were treated at the CVC for 1–10 days, with a median duration of 3 days. Weekend care at a partner clinic was recommended for 73% (82/113) of patients, and among those, 54% (44/82) attended at least one visit. The total number of treatment days (CVC and partner) ranged from 1 to 10 days (median = 4 days), and the total number of days receiving fluids in the clinic (CVC and partner clinic) ranged from 0 to 10 days (median = 2 days, n = 110). At-home fluid administration was prescribed in 81% (91/113) of cases. At-home fluid administration status was unknown for 24 dogs. Of those with known administration status, 85% (57/67) gave SQ fluids at home at least once. In addition to core protocol drugs, the treating veterinarian prescribed additional medications at their discretion (see Appendix 1).
Of the 113 included dogs, 73 survived, 23 died, two were euthanized during treatment, and 15 cases were LTF. LTF cases were not appreciably different from those with a known outcome on baseline factors; LTF dogs were slightly older (median of 4 months vs. 3 months, p = 0.053) and were less likely to have depressed mentation at baseline (p = 0.040). Of those dogs with a known outcome, 73/98 or 74% (95% CI, 65%–83%) survived.
Table 1 shows patient characteristics, history, baseline clinical and exam parameters, and treatment factors for survivors and non-survivors. Nine variables with p ≤ 0.25 in the bivariate analyses (Table 1) were included in logistic regression modeling. Total visit days, total fluid days, and visits to partner clinics were recoded for modeling. The final model is shown in Table 2. Dogs having ≥ 3 total number of clinic visits (relative to 1 or 2 visits) had greater odds of survival, while those requiring and receiving ≥ 2 total number of days of fluids (relative to 0 or 1 days), referred for and receiving weekend treatment at a partner clinic, and/or with pale mucous membrane color at baseline (relative to pink) had greater odds of non-survival. Hosmer–Lemeshow Chi-Square test supported adequate model fit, and the AUC suggested excellent ability to discriminate between survival and non-survival.17
Client survey
Overall, 53% (52/98) of dogs had an owner survey, with a greater percentage of survivors (60%, 44/73) than non-survivors (32%, 8/25). Sixty percent (31/52) of surveys were staff-administered, and 13% (7/52) of respondents completed the survey in Spanish. Of the owners who reported that their dog was prescribed medications for home, 96% (43/45) indicated that they mostly or completely understood how to administer them, and 87% (39/45) reported that administering them was easy or very easy (Table 3). Similarly, of those prescribed home fluids, 95% (42/44) reported that they mostly or completely understood how to administer them, and 84% (37/44) reported that administering them was easy or very easy. In open text responses, one client reported that fluids were difficult to give due to their disability, and another expressed discomfort with medical procedures despite receiving instruction. Another owner reported they could not get their dog to open his/her mouth. Ninety percent (46/51) of owners reported that bringing their dog to the clinic was easy or very easy to do. Only one cited challenges with transportation and work schedule. Almost all owners (98%, 50/51) agreed that they felt respected by the team and that the team genuinely cared about them and their pet, and all owners (100%, 51/51) reported being mostly or completely satisfied with the treatments their dog received.
| Treatment Aspect | No. | Not at all/Slightly | Somewhat | Mostly/Completely |
| Understood instructions | ||||
| *Medications | 45 | 0 | 2 (4%) | 43 (96%) |
| *Fluids | 44 | 1 (2%) | 1 (2%) | 42 (95%) |
| No. | Very hard/Hard | Neutral | Easy/Very easy | |
| Treatment easy/Difficult | ||||
| *Medications | 45 | 2 (4%) | 4 (9%) | 39 (87%) |
| *Fluids | 44 | 3 (7%) | 4 (9%) | 37 (84%) |
| Daily clinic visits | 51 | 1 (2%) | 4 (8%) | 46 (90%) |
| No. | Strongly disagree/Disagree | Neither agree nor disagree | Strongly agree/Agree | |
| Clinic experience | ||||
| Felt respected | 51 | 1 (2%) | 0 | 50 (98%) |
| Team cared about owner/pet | 51 | 1 (2%) | 0 | 50 (98%) |
| No. | Not at all/Slightly | Somewhat | Mostly/Completely | |
| Satisfaction with treatment | 51 | 0 | 0 | 51 (100%) |
| *Of owners who reported that their dog was prescribed fluids or medications for home; 7 owners reported no medications were prescribed for home, and 8 reported no fluids were prescribed for home. | ||||
Additional survey comments (n = 25) were analyzed for themes and sentiment to identify the shared experiences and opinions of the participants. The theme of professionalism was most frequently observed in the owner responses (10/25), describing the staff as helpful, kind, and informative. Half of the responses under the theme of professionalism focused on how well the staff kept them informed (n = 4). One owner wrote, ‘I feel the staff were very helpful and made it very clear the dog may or may not survive’. This quote demonstrates the importance of helping the owner be aware of the uncertainty and life-threatening nature of parvovirus. Another owner shared mutual support through staff professionalism and the information they provided, writing, ‘The process was terrifying but the staff were very informative and made the process easier to complete’. The sentiment analysis identified attitudes and experiences beyond the theme of staff professionalism, identifying that the majority (18/25) of owners found the treatment experience positive, sharing responses that expressed satisfaction or gratitude for the treatment of their dog. One owner shared direct gratitude for the care they personally received, writing, ‘Agradezco me atendieron con amor y empatía a mi dolor de ver tan enfermo mi pequeño perrito’ (I am grateful that they treated me with love and empathy for my pain of seeing my little dog so sick). One owner expressed neutral sentiment, writing ‘pet deceased’, and one owner shared a negative response, stating that the location of the partner clinic was not convenient. Three comments were not analyzed for themes or sentiment as their responses were ‘no’ or ‘none’.
Discussion
Study results support the success and feasibility of a lower-cost, once-daily clinic visit outpatient treatment for CPV. Seventy-four percent (73/98) of dogs treated with the protocol and with a known outcome survived. This is much higher than the <10% survival expected with no treatment,3 which is often the only alternative besides euthanasia when typical inpatient or alternative care is not accessible. Survival of 74% is also in line with survival reported in other outpatient (75% [95% CI, 66–82%] to 83% [95% CI, 74–90%])13–15 and inpatient (90% [95% CI, 68–99%])14 studies, even with only once-daily clinic visits. Extended monitoring, bloodwork, and other diagnostics, as well as rescue IV fluids and twice-daily appointments included in other outpatient protocols13,14 were not feasible for the CVC, which focuses primarily on high-volume preventative care and treatment for minor illnesses and conditions to serve as many pets and families as possible in the community. Despite these differences, the present study yielded results comparable to other reports, suggesting that the once-daily protocol is a reasonable option, particularly when more intensive care may not be accessible due to financial limitations, a lack of overnight care, or other barriers.
Understanding the predictors of survival in treatment studies is important for facilitating informed decision-making and guiding future research. Signalment and clinical signs such as male sex, small breed, low weight, fever, diarrhea, and indicators consistent with systemic inflammatory response syndrome have been associated with non-survival of CPV.18–21 However, studies are inconsistent, and information on prognostic indicators in outpatient treatment for CPV is limited. Venn et al.14 found potential associations between low weight and younger age and decreased survival, although these could not be statistically tested due to the small sample size. In the work of Perley et al.,13 a longer duration of clinical signs before treatment and weight gain during treatment were predictive of survival, and hypothermia was predictive of non-survival. Although the current study was unable to assess weight changes during treatment due to incomplete data on weight at the time of treatment conclusion, no associations were found between baseline weight, temperature, age, or duration of clinical signs, and survival outcome. Pale mucous membrane color on the initial exam, however, was associated with decreased survival. Membrane color may have been an indicator of either hypovolemic shock or anemia, both of which are associated with more severe cases of CPV.
There were three additional predictors of survival. Three or more clinic visits were associated with increased odds of survival, which may be due to the additional monitoring and/or treatments received. The number of visits could also serve as a proxy for other factors important for survival, such as owner compliance and/or the time to recovery. The association between greater number of clinic visits and survival could simply indicate that dogs that died did so early in treatment prior to three clinic visits. The exact date of symptom resolution or death was not consistently noted in the medical record, so examination of time to survival was not possible in this study. Horecka et al.18 reported an increased probability of survival after 5 days of treatment, and Magalhães et al.21 found that time hospitalized was greater among survivors (median of 5 days) compared to non-survivors (median of 3.5 days) in dogs with a clinical CPV diagnosis. Interestingly, needing and receiving two or more days of fluids in the clinic was associated with decreased survival, which may indicate that the patient was more severely affected. Subcutaneous fluids were not administered at every visit for all patients; if the patient was retaining fluid from an earlier treatment or was well-hydrated, fluids were withheld. While initial hydration status did not differ between survivors and non-survivors, it is possible that non-survivors were sicker upon presentation in a way not captured by the measured factors or that they did not recover as well or as quickly as survivors, requiring hydration support for a longer period. Receiving weekend care at the partner clinic was also associated with decreased survival, which may indicate that severely affected dogs were more likely to be referred for care and/or that their owners were more likely to bring them to the partner clinic. Unlike Sarpong and colleagues,15 the present study did not find that prescription of a caloric supplement (in this study, Nutrical) was associated with outcome. Inconsistencies in published predictors of survival are likely due to variations in the clinical presentation of dogs as well as the limited power to detect subtle differences between survivors and non-survivors in these studies. Additional research with larger sample sizes, consideration of other predictors, and repeated measures of indicators across the course of treatment are needed.
Owners are essential partners in veterinary medicine. It is crucial to consider a client’s circumstances, preferences, and perspectives in treatment decision-making to ensure the best possible outcome for patients and their families.22 While outpatient CPV treatment reduces the financial burden for owners, it requires more of their time and effort in the form of frequent clinic visits and at-home treatments, as well as an ability to recognize clinical signs, make decisions about and administer more complex treatments such as SQ fluids at home, which may not be possible for some. Results from this client survey, conducted at the end of the treatment, indicated that the great majority of clients (90%, 46/51) found the daily clinic visits highly manageable and were able to administer at-home treatments, including SQ fluids. This is further supported by data showing that 85% (57/67) of those prescribed at-home fluids were able to administer them to their dog at least once. Additionally, the survey results showed that nearly all clients felt cared for and respected and were highly satisfied with the treatment they received. Other research has also shown that clients receiving care at community veterinary medicine programs have a highly positive experience.23 Effective communication and the expression of empathy have been linked to higher client satisfaction and improved veterinarian–client relationships, which can positively influence treatment adherence and patient outcomes.24–27 Many owners seeking care at low-cost, subsidized clinics have not previously obtained veterinary care for their pets,23 and a positive first experience is crucial for increasing the likelihood that they will seek veterinary care in the future.23,28
The findings presented here are consistent with other research, which shows that less intensive, more affordable veterinary treatments for conditions such as pyometra and diarrhea have favorable outcomes.29–31 Spectrum of care (SoC) involves offering clients a range of diagnostic and treatment options for their pet, from basic, inexpensive to more technologically advanced, costly options grounded in evidence-based medicine and tailored to meet the needs and preferences of the individual pet patient and their family.32 SoC is one way to increase access to care for patients while facilitating trust and effective client–veterinarian partnerships.28 Outpatient CPV protocols offer an intermediate level of care along the continuum between hospitalization with intensive care and no treatment. Additionally, emerging treatments, such as monoclonal antibodies33–35 and fecal microbiota transplantation,36 have shown potential to reduce the severity and duration of clinical signs and improve outcomes in dogs with parvovirus; these may offer additional options for the treatment of CPV, although further research is needed to determine their effectiveness and feasibility in community or shelter practice. Veterinarians should understand the range of treatment options available for CPV, enabling them to identify the most suitable and feasible options for their patients, considering the severity of the animal’s clinical signs, available resources, and client circumstances and preferences, to increase access to treatment and facilitate good outcomes for their patients.
Strengths and limitations
The strengths of this research include its real-world community clinic implementation, prospective design, and measurement of client perspective. Nevertheless, certain study limitations warrant mention. As fecal samples were not typically available for dogs presenting with possible CPV, IDEXX Snap® Parvo tests were conducted via rectal swab, which is not consistent with product labeling and may have reduced test sensitivity.37 As a result, it is possible that CPV-positive dogs were incorrectly excluded from the study due to false negatives on the SNAP® Parvo Test. Also, outcomes were not known for 15 cases considered LTF. If a greater number of LTF cases did not return for treatment because they died at home or because they recovered, survival could have been overestimated or underestimated. However, 13% LTF is reasonable for this type of research, and a comparison of baseline factors for LTF and the sample with known outcomes revealed few differences, suggesting that LTF was likely not a significant threat to validity.
As is common with medical record research, data were sometimes inconsistent or incomplete, which limited the ability to examine other predictors of survival. There was no blood work or reliable data on other outcomes, such as time to resolution of clinical signs or mortality. These may be important to consider in future research for evaluating the cost–benefit of different treatment options. Furthermore, statistical power may have been lacking to detect associations between other potential predictors measured in this study and survival. The multivariable model examined nine independent variables in a stepwise process (the maximum number based on a general rule of thumb). The high odds ratios and wide CIs observed for some variables in the model may occur due to small sample sizes or skewed distributions, particularly when predictors are dichotomous. However, multivariable evaluation of the data provided valuable insights for future work. Finally, survey responses were available for only 53% of the sample, and this group was slightly overrepresented by owners of dogs who survived, who may be more likely to report a positive treatment experience compared to owners of dogs that did not survive.
Generalization
The findings may not generalize to all clinics or communities. While 90% of clients in the study reported that visiting the clinic once daily for treatments was easy, most lived in the surrounding neighborhood and, anecdotally, had access to a car. Clinic location and transportation are known barriers to care,11 and accessibility may be more challenging in communities where clients have a longer distance to travel, lack of access to transportation, and/or rely on public transportation. The CVC also provided services free of charge and arranged and paid for outpatient care at local private clinics when the CVC was closed. The feasibility of protocol implementation for other organizations or pet owners, particularly those with limited finances and limited access to nearby clinics, should be considered. One workaround is to send medications and fluids home for twice-daily, client-administered treatments during weekends and holidays as needed, as was done here when clients were unable to go to partner clinics. Additionally, after the protocol was implemented into a typical schedule at the CVC, informal staff feedback indicated that parvovirus treatment visits, especially the initial visit, could take longer than anticipated. Other clinics and shelters should ensure they have the necessary space and staff resources to implement an outpatient protocol safely and effectively and may need to adjust their clinic schedules to accommodate longer visits for CPV treatment cases. Finally, a few clients reported treatment challenges related to transportation difficulties, schedule conflicts, and difficulties administering fluids due to owner disability and dog behavior; these factors are important to discuss with clients when determining the feasibility and suitability of outpatient treatment.
Conclusion
Current findings indicate that a lower-cost, once-daily clinic outpatient protocol for the treatment of CPV is effective and feasible in a community veterinary medicine clinic setting, with 74% of the dogs treated with the protocol and with a known outcome surviving the disease. High client-reported adherence and satisfaction reinforce the protocol’s viability in real-world settings. As an alternative to an all-or-none approach to treating CPV, these findings build upon existing research to illustrate intermediate-level, evidence-based options for CPV treatment with good outcomes that can be tailored to the needs and preferences of the patient, client, clinic, and community. Clinics and shelters should consider the patient’s status, their resources to deliver the protocol, as well as potential client barriers (e.g., transportation challenges, ability and willingness to administer fluids at home) when determining if this protocol is the right fit for their setting and their patients.
This protocol has the potential to expand access to care for clients who lack financial resources, as well as for shelters and practices that lack in-house bloodwork capabilities and/or struggle with adequate staffing. This occurs by reducing the workload compared to hospitalization, allowing medical staff to spend more time caring for a larger number of patients. Given the data supporting positive outcomes, some owners may opt for outpatient care because they prefer to keep their pet at home or because of the pet’s reaction to being hospitalized.
Offering outpatient treatment as a part of a SoC approach, when appropriate, increases treatment access for more dogs with parvovirus, reducing unnecessary suffering, death, and euthanasia in affected dogs while keeping pets and families together. This also reduces moral distress in veterinary medical staff when they are unable to meet the needs of their patients. Veterinarians are encouraged to consider these findings when treating a wider variety of conditions with less expensive and less aggressive protocols based on data and their clinical experience and expertise to further expand access to care.
Author contributions
VA: conceptualization, methodology, formal analysis, writing-original draft
CB: conceptualization, methodology, writing-review and editing
MS1: conceptualization, methodology, formal analysis, writing-review and editing
CH: methodology, writing-review and editing
MS2: formal analysis, writing-review and editing
Acknowledgments
The authors thank the veterinarians, veterinary technicians and assistants, and clinic support staff at the ASPCA Miami Community Veterinary Clinic for administering the outpatient treatment protocol, capturing data in the medical record, and for providing feedback on the manuscript draft (Rachel Krieger, DVM; Magdalena Rodriguez, DVM). Special thanks to Caitlin Abreu and other patient liaisons at the clinic for administering the client survey and conducting follow-up calls for lost-to-follow-up cases. We also thank Samantha Brigham-Tress and Amanda Rodriguez for their technical assistance in accessing electronic medical record and partner clinic data, respectively.
Author notes
Preliminary results from this study were included in an oral presentation at the 2023 Access to Veterinary Care Virtual Conference.
References
| 1. | Blackwell MJ, O’Reilly A. Access to Veterinary Care – A National Family Crisis and Case for One Health. Adv Small Anim Care. 2023;4(1):145–157. doi: 10.1016/j.yasa.2023.05.003 |
| 2. | Access to Veterinary Care Coalition. Access to Veterinary Care: Barriers, Current Practices, and Public Policy. The University of Tennessee; 2018. |
| 3. | Njenga M, Nyaga P, Buoro I, Gathumbi P. Effectiveness of Fluids and Antibiotics as Supportive Therapy of Canine Parvovirus-2 Enteritis in Puppies. Bull Anim Health Prod Afr. 1990;38:379–389. |
| 4. | Prittie J. Canine Parvoviral Enteritis: A Review of Diagnosis, Management, and Prevention. J Vet Emergen Crit Care. 2004;14(3):167–176. doi: 10.1111/j.1534-6935.2004.04020.x |
| 5. | Goddard A, Leisewitz AL. Canine Parvovirus. Vet Clin North Am Small Anim Pract. 2010;40(6):1041–1053. doi: 10.1016/j.cvsm.2010.07.007 |
| 6. | Mazzaferro EM. Update on Canine Parvoviral Enteritis. Vet Clin North Am Small Anim Pract. 2020;50(6):1307–1325. doi: 10.1016/j.cvsm.2020.07.008 |
| 7. | Kelman M, Ward MP, Barrs VR, Norris JM. The Geographic Distribution and Financial Impact of Canine Parvovirus in Australia. Transbound Emerg Dis. 2019;66(1):299–311. doi: 10.1111/tbed.13022 |
| 8. | Park RM, Gruen ME, Royal K. Association between Dog Owner Demographics and Decision to Seek Veterinary Care. Vet Sci. 2021;8(1):1–19. doi: 10.3390/vetsci8010007 |
| 9. | PetSmart Charities, Gallup. State of Pet Care Study: Pet Parents’ Assessment of American Veterinary Care. 2025. Accessed May 14, 2025. https://www.gallup.com/analytics/659123/gallup-petsmart-charities.aspx |
| 10. | King E, Mueller MK, Dowling-Guyer S, McCobb E. Financial Fragility and Demographic Factors Predict Pet Owners’ Perceptions of Access to Veterinary Care in the United States. J Am Vet Med Assoc. 2022;260(14):1–8. doi: 10.2460/javma.21.11.0486 |
| 11. | LaVallee E, Mueller MK, McCobb E. A Systematic Review of the Literature Addressing Veterinary Care for Underserved Communities. J Appl Anim Welf Sci. 2017;20(4):381–394. doi: 10.1080/10888705.2017.1337515 |
| 12. | Pasteur K, Diana A, Yatcilla JK, Barnard S, Croney CC. Access to Veterinary Care: Evaluating Working Definitions, Barriers, and Implications for Animal Welfare. Front Vet Sci. 2024;11:1335410. doi: 10.3389/fvets.2024.1335410 |
| 13. | Perley K, Burns CC, Maguire C, et al. Retrospective Evaluation of Outpatient Canine Parvovirus Treatment in a Shelter–Based Low–Cost Urban Clinic. J Vet Emergen Crit Care. 2020;30(2):202–208. doi: 10.1111/vec.12941 |
| 14. | Venn EC, Preisner K, Boscan PL, Twedt DC, Sullivan LA. Evaluation of an Outpatient Protocol in the Treatment of Canine Parvoviral Enteritis. J Vet Emergen Crit Care. 2017;27(1):52–65. doi: 10.1111/vec.12561 |
| 15. | Sarpong KJ, Lukowski JM, Knapp CG. Evaluation of Mortality Rate and Predictors of Outcome in Dogs Receiving Outpatient Treatment for Parvoviral Enteritis. J Am Vet Med Assoc. 2017;251(9):1035–1041. doi: 10.2460/javma.251.9.1035 |
| 16. | StataCorp. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC; 2021 |
| 17. | Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 1st ed. Wiley; 2013. doi: 10.1002/9781118548387 |
| 18. | Horecka K, Porter S, Amirian ES, Jefferson E. A Decade of Treatment of Canine Parvovirus in an Animal Shelter: A Retrospective Study. Animals. 2020;10(6):939. doi: 10.3390/ani10060939 |
| 19. | Chalifoux NV, Parker SE, Cosford KL. Prognostic Indicators at Presentation for Canine Parvoviral Enteritis: 322 Cases (2001–2018). J Vet Emergen Crit Care. 2021;31(3):402–413. doi: 10.1111/vec.13052 |
| 20. | Kalli I, Leontides LS, Mylonakis ME, Adamama-Moraitou K, Rallis T, Koutinas AF. Factors Affecting the Occurrence, Duration of Hospitalization and Final Outcome in Canine Parvovirus Infection. Res Vet Sci. 2010;89(2):174–178. doi: 10.1016/j.rvsc.2010.02.013 |
| 21. | Magalhães TR, Gregório H, Araújo J, et al. Prognostic Factors Associated with Survival and Hospitalization Time in Pediatric Canine Patients Diagnosed with Presumptive Acute Viral Gastroenteritis. Vet World. 2022;15(8):2095–2101. doi: 10.14202/vetworld.2022.2095-2101 |
| 22. | Brown CR, Edwards S, Kenney E, et al. Family Quality of Life: Pet Owners and Veterinarians Working Together to Reach the Best Outcomes. J Am Vet Med Assoc. 2023;261(8):1238–1243. doi: 10.2460/javma.23.01.0016 |
| 23. | Kogan LR, Accornero VH, Gelb E, Slater MR. Community Veterinary Medicine Programs: Pet Owners’ Perceptions and Experiences. Front Vet Sci. 2021;8:678595. doi: 10.3389/fvets.2021.678595 |
| 24. | McArthur M, Fitzgerald J. Companion Animal Veterinarians’ Use of Clinical Communication Skills. Aust Veterinary J. 2013;91(9):374–380. doi: 10.1111/avj.12083 |
| 25. | Janke N, Shaw JR, Coe JB. On-Site Communication Skills Education Increases Appointment-Specific Client Satisfaction in Four Companion Animal Practices in Texas. J Am Vet Med Assoc. 2022;260(13):1711–1720. doi: 10.2460/javma.22.06.0242 |
| 26. | Kanji N, Coe JB, Adams CL, Shaw JR. Effect of Veterinarian-Client-Patient Interactions on Client Adherence to Dentistry and Surgery Recommendations in Companion-Animal Practice. J Am Vet Med Assoc. 2012;240(4):427–436. doi: 10.2460/javma.240.4.427 |
| 27. | Stackhouse N, Chamberlain J, Bouwer A, Mexas AM. Development and Validation of a Novel Measure for the Direct Assessment of Empathy in Veterinary Students. J Vet Med Educ. 2020;47(4):452–464. doi: 10.3138/jvme.0818-096r |
| 28. | Brown CR, Garrett LD, Gilles WK, et al. Spectrum of Care: More than Treatment Options. J Am Vet Med Assoc. 2021;259(7):712–717. doi: 10.2460/javma.259.7.712 |
| 29. | Pailler S, Slater MR, Lesnikowski SM, et al. Findings and Prognostic Indicators of Outcomes for Bitches with Pyometra Treated Surgically in a Nonspecialized Setting. J Am Vet Med Assoc. 2022;260(S2):S49–S56. doi: 10.2460/javma.20.12.0713 |
| 30. | Pailler S, Slater MR, Lesnikowski SM, et al. Findings and Prognostic Indicators of Outcomes for Queens with Pyometra Treated Surgically in a Nonspecialized Hospital Setting. J Am Vet Med Assoc. 2022;260(S2):S42–S48. doi: 10.2460/javma.20.12.0712 |
| 31. | Bryan CE, Cade JC, Mackin AJ, Sullivant AM. Evaluation of a Structured Individualised Protocol as a Potential Cost–Effective Diagnostic and Therapeutic Approach to Chronic Diarrhoea in the Dog. Vet Med Sci. 2019;5(2):210–221. doi: 10.1002/vms3.154 |
| 32. | Stull JW, Shelby JA, Bonnett BN, et al. Barriers and Next Steps to Providing a Spectrum of Effective Health Care to Companion Animals. J Am Vet Med Assoc. 2018;253(11):1386–1389. doi: 10.2460/javma.253.11.1386 |
| 33. | Elanco US Inc. Canine Parvovirus Monoclonal Antibody Product Label. 2023. Accessed Feb 10, 2025. https://assets-us-01.kc-usercontent.com/e4748d51-2c24-00f7-fc54-65f3864ee8b1/af9cbb69-e26d-4a06-b0c8-b9ec99593929/Canine%20Parvovirus%20Monoclonal%20Antibody%20PROMO_WEB_103743Asa_PA103743A_W2a%2011.20.24.pdf |
| 34. | Larson L, Miller L, Margiasso M, et al. Early Administration of Canine Parvovirus Monoclonal Antibody Prevented Mortality after Experimental Challenge. J Am Vet Med Assoc. 2024;262(4):506–512. doi: 10.2460/javma.23.09.0541 |
| 35. | Welton M, Hadden H, Herron ME, Winston JA. Clinical Efficacy of Canine Parvovirus Monoclonal Antibody for Naturally Occurring Parvovirus in a Shelter Setting. Presented at the International Society for Companion Animal Infectious Diseases (ISCAID) Symposium; October; Vancouver; 2024. |
| 36. | Pereira GQ, Gomes LA, Santos IS, Alfieri AF, Weese JS, Costa MC. Fecal Microbiota Transplantation in Puppies with Canine Parvovirus Infection. J Vet Intern Med. 2018;32(2):707–711. doi: 10.1111/jvim.15072 |
| 37. | IDEXX Laboratories, Inc. SNAP Parvo Test Product Insert. 2022. Accessed Jul 14, 2025. https://www.idexx.com/files/snap-parvo-pkg-insert-en.pdf |
Appendix 1: Once-daily outpatient treatment protocol for canine parvovirus
- Canine Parvovirus Positive Patient Identified:
- Clinical signs consistent with a diagnosis of canine parvovirus (i.e., sudden onset vomiting, diarrhea, inappetence and/or lethargy).
- IDEXX SNAP® Parvo test positive (rectal swab).
- Triage Patient:
- Patients that are not in hypovolemic shock (defined below) will be offered the outpatient protocol.
- Hypovolemic shock is defined as having 5 or more of the following criteria:
- Cold extremities
- Dehydration > 8%
- Poor pulse quality
- Heart rate > 180 bpm
- Capillary refill time (CRT) >2 s
- Obtunded/stuporous mentation
- Temperature > 39.4ºC (103.0ºF) or < 36.7ºC (98.0ºF)
- Hypovolemic shock is defined as having 5 or more of the following criteria:
- Patients who present in hypovolemic shock may be:
- Referred to a full-service veterinary hospital
- Offered euthanasia
- Patients that are not in hypovolemic shock (defined below) will be offered the outpatient protocol.
- Outpatient Treatment Information for Owners:
- Once-daily clinic visits for an average of 3–4 days (may be shorter or longer).
- At-home SQ fluids – owner will receive instructions and supplies.
- At-home oral medications for treatment days when the clinic is closed.
- At-home monitoring.
- Keep the patient clean, dry, warm, quiet.
- Keep track of everything- ins and outs.
- Feeding:
- Offer boneless skinless boiled chicken and rice or prescribed diet.
- Do not force-feed.
- Free access to water:
- Supplement with plain Pedialyte.
- Do not force the patient to drink.
- Must be kept inside:
- No walks or going in the yard.
- Sanitize the house, clothes, bedding, and soiled linens using a 1:30 bleach solution.
- Discuss contagiousness to other dogs.
- Isolate from other dogs in the house/neighborhood.
- Fecal shedding 4 weeks.
- Survival in the environment for 5–7 months.
- Recommend DA2PP vaccines when recovered.
- Initial Outpatient Treatments:
- Convenia (cefovecin): 8 mg/kg SQ
- Pyrantel pamoate (if not vomiting): 10 mg/kg (0.1 mL/lb) PO
- Cerenia (maropitant): 1 mg/kg SQ
- Famotidine (if not eating): 1 mg/kg SQ
- Crystalloid fluid therapy
- AM visit: 40mL/kg (adjust as needed by attending DVM)
- PM visit: 60mL/kg (adjust as needed by attending DVM)
- Buprenorphine: 0.02 mg/kg SQ if the patient is experiencing abdominal pain (whining on expiration, irregular shallow breathing, abdominal guarding and tenderness)
- Instruction on administering SQ fluids at home and dispense supplies
- Follow-up Once Daily Outpatient Visits:
- History:
- Progress.
- Food/water intake.
- Eliminations.
- Vomiting.
- Physical Exam.
- Evaluate the patient’s progress:
- If signs are resolving, withhold all medications and fluids and evaluate for ‘Recovery’ in 24 h as defined below.
- If stable with continuing signs, continue treatments.
- If the patient’s condition deteriorates, jump to ‘Failure to Respond to Treatment’ section below.
- Treatments Monday through Friday (when CVC is open):
- Morning Treatments at the CVC
- Cerenia (maropitant): 1 mg/kg SQ SID.
- If the patient is not adequately responding to Cerenia, Zofran (ondansetron) may be given at 0.5mg/kg sublingual q 8 h
- Famotidine (if not eating): 1 mg/kg SQ SID.
- Crystalloid fluid therapy:
- 40mL/kg (adjust as needed by attending DVM)
- If part or all of the previous dose of SQ fluids remains at the next treatment, give partial dose of SQ fluids (subjectively determined) or withhold additional SQ fluids.
- Buprenorphine: 0.02 mg/kg SQ if the patient is experiencing abdominal pain (whining on expiration, irregular shallow breathing, abdominal guarding and tenderness).
- Schedule next treatment.
- Cerenia (maropitant): 1 mg/kg SQ SID.
- Evening treatment at home to be administered by owner:
- Crystalloid SQ fluid therapy – as directed.
- Morning Treatments at the CVC
- Treatments on Sunday, Monday, and other days on which the CVC is closed:
- If the patient is referred to a partner clinic
- Cerenia (maropitant): 1 mg/kg SQ SID.
- If the patient is not adequately responding to Cerenia, Zofran (ondansetron) may be given at 0.5mg/kg sublingual q 8 h.
- Famotidine (if not eating): 1 mg/kg SQ SID.
- Crystalloid fluid therapy:
- 40mL/kg (adjust as needed by attending DVM)
- If part or all of the previous dose of SQ fluids remains at the next treatment, give partial dose of SQ fluids (subjectively determined) or withhold additional SQ fluids.
- Buprenorphine: 0.02 mg/kg SQ if the patient is experiencing abdominal pain (whining on expiration, irregular shallow breathing, abdominal guarding and tenderness).
- Schedule the next treatment at a partner clinic or CVC.
- Evening treatment at home to be administered by the owner:
- Crystalloid SQ fluid therapy – as directed.
- Cerenia (maropitant): 1 mg/kg SQ SID.
- If the owner will be providing all treatment at home on days that CVC is closed:
- Crystalloid SQ fluid therapy – twice daily as directed
- Oral Cerenia (maropitant): 2 mg/kg PO SID or Zofran (ondansetron) at 0.5mg/kg sublingual q 8 h
- Oral Famotidine (if not eating): 1 mg/kg PO BID
- Crystalloid SQ fluid therapy – twice daily as directed
- If the patient is referred to a partner clinic
- Discretionary treatments at the CVC or private partner clinics included other/additional antibiotics, dewormers, stomach protectants, antihistamines, steroids, NSAIDs, antidepressants, and vitamin B.
- History:
- Recovery – Established by final recheck or phone conversation with owner:
- Resolution of vomiting for 24 h.
- Return of stool to normal consistency.
- Return of appetite.
- Normal energy level.
- Failure to Respond to Treatment:
- Defined by:
- Development of neurological symptoms (seizures, inappropriate vocalization).
- Suspicion of aspiration pneumonia.
- Intussusception.
- Decline in mentation to stuporous/obtunded.
- Decline in body condition, based on physical examination findings.
- No interest in eating or drinking.
- Uncontrolled hemorrhagic diarrhea.
- Intractable emesis.
- Dehydration >10% for two consecutive appointments.
- Once it is determined the patient has failed the Outpatient Protocol, the attending veterinarian recommends the patient continue more intensive treatment in an inpatient setting or be humanely euthanized.
- Defined by:
Appendix 2: Canine parvovirus outpatient treatment client survey
This short survey will ask about your experience with the treatment for the illness that caused vomiting and/or diarrhea in your dog (canine parvovirus). Your answers will help us improve the treatment for other dogs and their families in the future.
Fluids
How well did you understand the instructions about how to give fluids under the skin to your dog at home?
NA-the veterinarian didn’t give me any fluids for home
1-Not at all 2-Slightly 3-Somewhat 4-Mostly 5-Completely
1b. [if < Mostly] Tell us more. Which parts were hard to understand? What might we have done better to help you? [open text]
How easy was it to give fluids under the skin to your dog at home as instructed?
NA- the veterinarian didn’t give me any fluids for home
1-Very Hard 2-Hard 3-Neutral 4-Easy 5-Very Easy
2b. [if Hard or Very Hard] Tell us exactly what was hard for you. [open text]
Medications
3. How well did you understand the instructions about how to give medications to your dog at home?
NA- the veterinarian didn’t give me any medications for home
1-Not at all 2-Slightly 3-Somewhat 4-Mostly 5-Completely
3b. [if < Mostly] Tell us more. Which parts were hard to understand? What might we have done better to help you? [open text]
4. How easy was it to give medications to your dog at home as instructed?
NA- the veterinarian didn’t give me any medications for home
1-Very Hard 2-Hard 3-Neutral 4-Easy 5-Very Easy
4b. [if Hard or Very Hard] Tell us what exactly was hard for you. [open text]
Clinic Visits
5. How many times, including your first visit for this illness, did you bring your dog to the clinic for treatment of this illness?
1 2 3 4 5 6 7 8 or more times
6. How easy was it to bring your dog to the clinic every day for checkups?
1-Very Hard 2-Hard 3-Neutral 4-Easy 5-Very Easy
6b. [if Hard or Very Hard] Tell us exactly what was hard for you. [open text]
7. Thinking about all your visits to the clinic. How much do you agree with the following statements:
7a. I felt respected by the team providing treatment for my pet.
1-Strongly Disagree 2-Disagree 3-Neither Agree nor Disagree 4-Agree 5-Strongly Agree
7b. I believe the treatment team genuinely cares about me and my pet.
1-Strongly Disagree 2-Disagree 3-Neither Agree nor Disagree 4-Agree 5-Strongly Agree
8. How satisfied are you with the overall treatment your dog received (both the treatment given in the clinic and at home)?
1-Not at all 2-Slightly 3-Somewhat 4-Mostly 5-Completely
9. Anything more you would like to tell us about your answers above or your experience with the treatment for this illness (canine parvovirus) in your dog?
[open text]